The Achilles tendon is a large tendon at the back of the lower leg and ankle that connects the calf muscles to the heel. It is the largest tendon in the body, and its strength allows us to push off with forces up to 10 times our body weight.
Achilles Tendon Tear
An Achilles tendon tear, or rupture, usually is a complete gap between the upper and lower portions of this tendon. It most often occurs 2-3 inches above the heel bone but can be directly at the attachment or higher in the leg.
Symptoms
A tear usually occurs during activities such as running and jumping, or trauma such as a slip and fall. Most patients report their first feeling was a “pop” or like they were struck in the back of the ankle, followed by some pain. There often is no pain in this area before the actual tear. After the tear, patients complain of weakness when pushing off of their foot during walking or when trying to stand on tiptoe.
Diagnosis
Your foot and ankle orthopedic surgeon often performs an examination to make a diagnosis. You will lie in a facedown position with your ankles off the edge of the exam table. When the Achilles tendon is not torn, it is taut and the ankle lies in a toe down position of approximately 20 degrees. Squeezing the upper calf will cause the toes to point down even further.
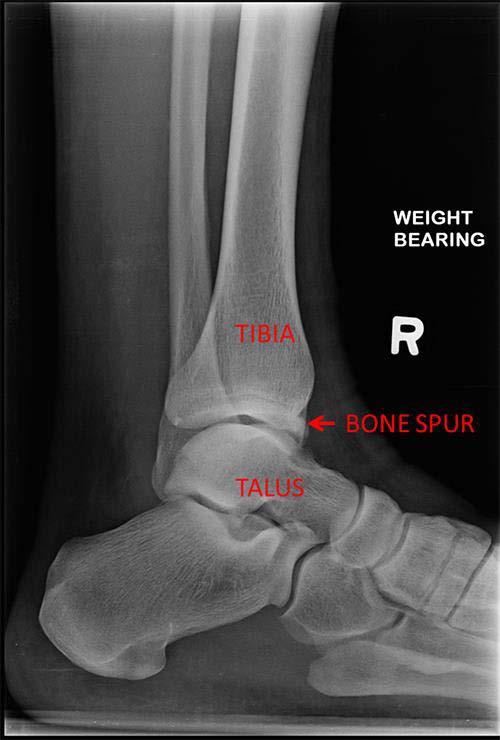
If the tendon is torn, it does not have this tension and the ankle usually will hang at about a 90-degree angle. Squeezing the upper calf will cause weak or no movement. Special tests such as ultrasound, X-rays, and MRI scans typically are not required but can be in some instances.
Treatments
At first, the leg is placed at rest in a splint or special boot. It is important to see a foot and ankle orthopedic surgeon soon after the injury so the best treatment can be started within a few days.
Both non-surgical and surgical treatments have been well studied but remain debated. In general, surgical treatment is thought to give greater strength and result in a lower risk of repeat tear. However, surgery has an increased risk of wound healing problems, nerve damage, and infection plus the usual risks associated with surgery. Blood clots are a concern with both types of treatment. Your foot and ankle orthopedic surgeon will be the best person to guide you through the pros and cons and help you to select the best option.
Non-surgical Treatment
Non-surgical treatment starts with a period of rest in a boot for the injured leg. You will need to use crutches, a walker, or wheelchair in order to not put weight on the leg. Within the first few weeks you will start doing active motion. Gradually, you will be allowed to put weight on the leg and start specific strengthening exercises. The length of treatment may be different for each patient but usually takes about three months. It is often guided by a physical therapist along with the orthopedic surgeon.
Surgical Treatment
In this surgery, your foot and ankle orthopedic surgeon will place stitches into the tendon above and below the area of the tear and then pull the ends together. The surgery often is performed through a very small incision to minimize the risk of wound complications. The recovery after surgery is similar to the non-surgical treatment but can be slightly shorter.
Recovery
Since tendons do not have a great blood supply, healing is a slow process. Patients usually can start light jogging in 3-6 months with return to sports involving cutting and jumping in 6-9 months. Full return of strength and the feeling of being normal may take more than a year.
FAQs
After an Achilles tendon tear, how likely am I to tear the other side?
About 6% of patients with an Achilles tendon tear will have the same injury in the other foot.
Is there anything I can do to make the tendon heal faster?
Starting range-of-motion exercises and putting weight on the injured leg early have shown better results than long periods of immobilization on crutches. However, it has to be balanced by the risk of pulling apart the ends of the tendon if you stretch too much too early. Stopping smoking for at least a few months while the tendon heals also is likely to be of benefit.