What is a Dislocated Elbow?
When the joint surfaces of an elbow are separated, the elbow is dislocated. Elbow dislocations can be complete or partial. In a complete dislocation, the joint surfaces are completely separated (Figure 1a). In a partial dislocation, the joint surfaces are only partly separated. A partial dislocation is also called a subluxation (Figure 2).



The elbow is stable due to bone surfaces, ligaments (which connect bones) and muscles. When an elbow dislocates, all of these can be injured to different degrees. A simple dislocation does not have any major bone injury. A complex dislocation can have severe bone and ligament injuries (Figure 3). In the most severe dislocations, there is injury to the blood vessels and nerves that travel across the elbow. If this happens, there is a risk of losing the arm.

Three bones come together to make up the elbow joint (Figure 4). The humerus bone is in the upper part of the arm and attaches to the two bones of the forearm (ulna and radius). Each of these bones has a very distinct shape. Ligaments connect all three bones together. As muscles contract and relax, two unique motions can occur at the elbow:
- Bending occurs through a hinge joint that allows you to bend and straighten the elbow.
- Rotation occurs though a ball and socket joint that allows the hand to be rotated palm up and palm down.
Injuries and elbow dislocations can affect either of these motions.
Elbow dislocations are uncommon. The most common age for an elbow dislocation is 30 years old.
Mechanism of Injury
Elbow dislocations typically occur when a person falls onto an outstretched hand. When the hand hits the ground, the force is sent to the elbow. Usually there is a turning motion in this force. This can drive and rotate the elbow out of its socket. Elbow dislocations can also happen in car accidents.
When the crash happens, the passengers often reach forward to cushion the impact. The force sent through the arm can dislocate the elbow, just as in a fall.
Diagnosis
When the elbow is dislocated, the deformity of the arm is obvious. X-rays are the best way to confirm that the elbow is dislocated. If the bone detail is difficult to evaluate on an X-ray, sometimes a computer tomography (CT) scan will be done. If it is important to evaluate the ligaments, a magnetic resonance imaging (MRI) can be helpful.
However, the doctor will set the elbow first, without waiting for the CT scan or MRI. These studies are usually taken after the dislocated elbow has been put back in place.
Risk Factors and Prevention
Some people are born with greater laxity or looseness in their ligaments. These people are at greater risk for dislocating their elbows. Some people are born with an ulna bone that has a shallow groove for the elbow hinge joint. They have a slightly higher risk for dislocation. Nothing can be done to alter these risk factors.
Symptoms of a Dislocated Elbow
A complete elbow dislocation is extremely painful and very obvious. The arm will look deformed and may have an odd twist at the elbow. Get emergency treatment. It is important to evaluate the circulation of the arm and to check pulses at the wrist after an elbow dislocation.
If the artery is injured at the time of dislocation, the hand will be cool to touch and may have a white or purple hue. This is due to the lack of warm blood getting to the hand. It is also important to check the nerve supply to the hand.
If nerves have been injured during the dislocation, some or all of the hand may be numb and not able to move. Further testing such as an X-ray is necessary to determine if there is a bone injury. X-rays can also help show the direction of the dislocation.
A partial elbow dislocation or subluxation can be harder to detect. Typically it happens after an accident, but because the elbow is only partially dislocated, the bones can spontaneously relocate and the joint may appear fairly normal. There may be pain, however. The elbow will usually move fairly well.
There may be bruising on the inside and outside of the elbow where ligaments may have been stretched or torn. Partial dislocations can recur on a chronic basis if the ligaments never heal.
Treatment Options: Nonsurgical
The goal of immediate treatment of a dislocated elbow is to put the elbow back in joint. The long term goal is to restore function to the arm. First the alignment of the elbow must be restored. This can usually be done in an emergency department. The patient will receive sedation and pain medications. The act of restoring alignment at the elbow is called a reduction maneuver (Figure 1b). This should be done gently and slowly and usually takes two people to perform.
Simple elbow dislocations are treated with early motion after a short period in a splint or sling. Keeping the elbow immobile for a long time usually results in poor range of motion for the recovered elbow. Physical therapy can be helpful during this period of recovery. Some people will never recover full elbow extension even after a course of therapy.
Fortunately the elbow can work very well even without full motion. Once the elbow’s range of motion improves, the doctor or physical therapist may add a strengthening program. Interval X-rays may be necessary while the elbow recovers. This helps to ensure that the elbow joint remains well aligned.
Treatment Options: Surgical
In a complex elbow dislocation, surgery may be necessary to restore bone alignment and repair ligaments. It can be difficult to reduce the joint and to keep it in line. There is an increased risk for arthritis in the joint if:
- The alignment of the bones is not good.
- The elbow does not track well.
- The elbow continues to dislocate.
After the surgery, the elbow may be protected with an external hinge. This device guards against re-dislocation. If there are associated blood vessel or nerve injuries with the elbow dislocation, multiple surgeries may be necessary. These surgeries repair the blood vessels and nerves in addition to reducing the joint. They also fix the bone and ligament injuries.
Research on the Horizon/What’s New?
Treatment for simple dislocations is usually straightforward and the results are usually good. However, many people with complex dislocations still end up with permanent disability at the elbow. Treatment is evolving to improve results for these people.
The best time to schedule surgery is being evaluated for treatment of complex dislocations. For some patients with complex dislocations, it seems that a slight delay for definitive surgery may improve results by allowing swelling to decrease.
The dislocation still needs to be reduced right away, but then a brace, splint or external fixation frame may rest the elbow for about a week before a specialist surgeon attempts major reconstructive surgery.
Moving the elbow early appears to be good for recovery for both kinds of dislocations. However, early movement with complex dislocations can be difficult. Pain management techniques encourage early movement. Improved therapy and rehabilitation techniques such as continuous motion machines, dynamic splinting (spring-loaded assist devices) and progressive static splinting can improve results.
Late reconstructive surgery can successfully restore motion to some stiff elbows. This surgery removes scar tissue and extra bone growth. It also removes obstacles to movement.
Severe arthritis can develop in the elbow. For this condition, newly designed elbow replacement prosthesis can be implanted. The arthritic elbow joint can be replaced with an artificial elbow, similar to joint replacements in the hip or knee. This decreases pain and improves motion.





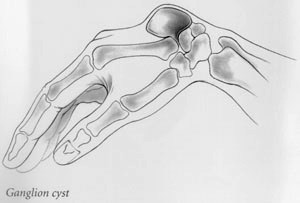 These treatments leave the outer shell and the stalk of the ganglion intact, so it may reform and reappear. Outpatient surgery can remove the ganglion, but is no guarantee that the cyst will not recur. Part of the involved joint capsule or tendon sheath may also be removed.
These treatments leave the outer shell and the stalk of the ganglion intact, so it may reform and reappear. Outpatient surgery can remove the ganglion, but is no guarantee that the cyst will not recur. Part of the involved joint capsule or tendon sheath may also be removed.