Arthroscopy is the medical term for a procedure that our orthopedic specialists use to examine, diagnose, and repair problems inside your shoulder joint. This word comes from two separate Greek words, “arthro” meaning “joint” and “skopein” meaning “to look.” This term means “to look within the joint.”
How do I plan for a shoulder arthroscopy?
Your orthopedic specialist may ask you to see your family doctor to make sure that you do not have any health concerns that should be addressed before your procedure. You may need to have an electrocardiogram, blood tests, and a chest X-ray before your surgery. If you have any health risks, you should discuss this with the surgeon and advise him of any medications or supplements that you are currently taking.
If you are in fairly good health, your shoulder arthroscopy will most likely be performed on an outpatient basis. The surgical center will contact you before the procedure to discuss the specific details. Make sure you follow their instructions regarding arrival time and when to stop eating or drinking prior to your operation.
Before your shoulder arthroscopy, a member of the anesthesia team will discuss your anesthesia options. Most shoulder arthroscopic procedures are performed using regional nerve blocks, which numb your arm and shoulder. The numbing medicine will be injected in the base of your neck or high upon your shoulder. The nerves that control feeling in your shoulder and arm will be targeted so you do not feel anything during the operation and for several hours after your surgery to help with post-operative discomfort.
Many of our orthopedic specialists combine nerve blocks with sedation or a general anesthetic in order to make you comfortable while lying on the operating table. Most shoulder arthroscopies take less than one hour; however, the length of your surgery will depend on what the doctor finds and what repairs are necessary.
Before you undergo a shoulder arthroscopy, plan to wear comfortable clothing that is easy to put on and take off. You should also leave all watches, jewelry, and valuables at your residence. You will also have to arrange to have someone drive you home after your procedure. Plan for assistance for at least two weeks following your shoulder arthroscopy, as tasks at home may be a little difficult.
What happens during a shoulder arthroscopy?
Once you have arrived and are positioned in the surgical room, you will be placed in the beach chair position. This is a semi-seated position to allow you to be essentially reclining in a chair. The surgical team will remove the hair from the operative site if necessary, and then spread an antiseptic solution on your shoulder to properly cleanse and sterilize the surgical site. The shoulder and arm will be covered with sterile drapes, and your arm will be placed in a holding device to keep it safe and stable.
The orthopedic specialist will first inject fluid into one of the small incisions he makes on your shoulder. This makes it easier for him to insert the instruments that will be used to visualize the structures with the arthroscope. Images from this scope are projected on a TV monitor so the surgeon can see inside your shoulder clearly.
Fluid flows through the arthroscope as he guides it around the joint space of the shoulder. Once your problem is identified, the orthopedic specialist can insert tiny instruments through the buttonhole-sized incisions for the purpose of removal or repair. These specialized instruments are necessary for tasks such as cutting, suture passing, knot tying, or shaving. Once the procedure is complete, the surgeon will close these incisions with stitches or Steri-strips and cover that will a large, soft bandage.
What should I expect after my shoulder arthroscopy?
During the recovery period, you will stay in a recovery room for a couple of hours before being discharged home. The orthopedic specialist and his team will monitor your condition to make sure you are ready to travel. At home, you can expect some pain and discomfort for a least a week following the procedure. Ice is recommended to help with this and your doctor may prescribe you some medication. You are allowed to shower once your wounds are no longer draining, but should avoid prolonged soaking or scrubbing of the incisions. A special immobilizer will be issued for the purpose of protecting your shoulder. The doctor will advise you on how long this will be needed.
Rehabilitation will allow you to get back to your daily activities. This is an exercise program to help you regain your range of motion and strength in your shoulder. It is important for you to follow doctor’s orders and make a noble effort at your rehabilitation in order for full recovery to occur.



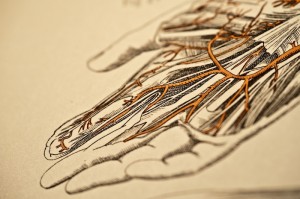 We see many patients who have lumps and bumps in their hand that are painful, growing, affect function, and are often worry some for the patient due to the concern for cancer. If you are concerned about a hand tumor, wrist mass, or finger cyst, you should schedule a consultation to put your mind at ease with a diagnosis and to discuss treatments available.
We see many patients who have lumps and bumps in their hand that are painful, growing, affect function, and are often worry some for the patient due to the concern for cancer. If you are concerned about a hand tumor, wrist mass, or finger cyst, you should schedule a consultation to put your mind at ease with a diagnosis and to discuss treatments available.