Description
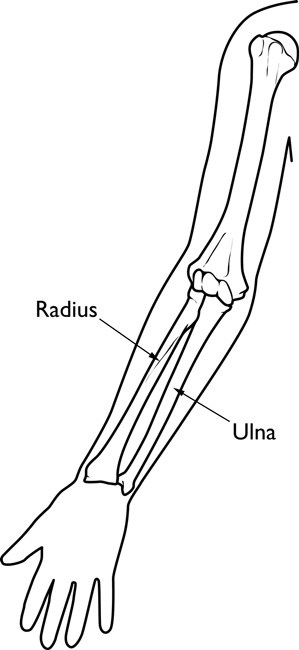
The bones of the forearm are the radius and the ulna. If you hold your arm naturally by your side, the ulna is the bone closer to you and the radius is farther away.
Fractures of the forearm can occur near the wrist at the farthest (distal) end of the bone, in the middle of the forearm, or near the elbow at the top (proximal) end of the bone.
A child’s bones are also subject to a unique injury called a growth plate fracture. Growth plates are made of cartilage near the ends of children’s bones. They help determine the length and shape of the mature bone.
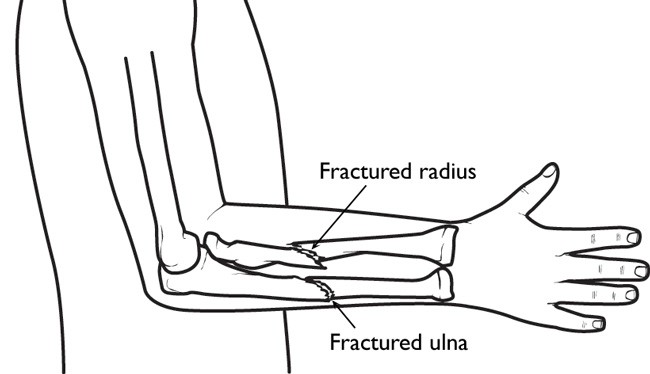
Fractures of both bones in the forearm.
Fractures in a child’s bones begin to heal much more quickly than an adult’s bones. If you suspect a fracture, you should obtain prompt medical attention for the child so that the bones can be set for proper healing.
Statistics
Forearm fractures account for 40% to 50% of all childhood fractures. About three out of four forearm fractures in children involve the wrist-end of the radius.
Cause
Children love to run, hop, skip, jump and tumble. But if a child falls onto an outstretched arm, he or she might break one or both of the bones in the forearm.
Classifications
Torus fracture. This is also called a “buckle” fracture. The topmost layer of bone on one side of the bone is compressed, causing the other side to bend away from the growth plate. This is a stable fracture and the broken pieces of bone have not separated apart (displaced).
Metaphyseal fracture. The fracture is across the upper, or lower, portion of the shaft of the bone and does not affect the growth plate.
Greenstick fracture. The fracture extends through a portion of the bone, causing it to bend on the other side.
Galeazzi fracture. The injury affects both bones of the forearm. There is usually a displaced fracture in the radius and a dislocation of the ulna at the wrist, where the radius and ulna come together.
Monteggia fracture. The injury affects both bones of the forearm. There is usually a fracture in the ulna and the top (head) of the radius is dislocated. This is a very severe injury and requires urgent care.
Growth plate fracture. Also called a physeal fracture, this fracture occurs at or across the growth plate. Usually these fractures affect the growth plate of the radius near the wrist.
Symptoms
In most cases, a broken forearm causes severe pain. Your child’s forearm and hand may also feel numb.
Examination, Signs
This child’s forearm fracture has resulted in a bent appearance of the forearm.
(Courtesy of Texas Scottish Rite Hospital for Children)
- Any type of deformity about the elbow, forearm, or wrist
- Tenderness
- Swelling
- An inability to rotate or turn the forearm
Your doctor will also test to make sure that the nerves and circulation in your child’s hand and fingers have not been affected.
Investigation, Tests
The hand, wrist, arm, and elbow can all be injured during a fall on an outstretched arm. To determine exactly what injuries have occurred, your doctor will probably want to see x-rays of the elbow and wrist, as well as the forearm.
Nonsurgical Treatment
Treatment depends on the type of fracture and the degree of displacement.

Casts support and protect broken bones while they heal.
Some mild fractures, such as buckle fractures, may simply need the support of a splint or cast until they heal. For more severe fractures that have become angled, your doctor may be able to push (manipulate) the bones into proper alignment without surgery, as long as the bones have not broken through the skin.
A stable fracture, such as a buckle fracture, may require 3 to 4 weeks in a cast. A more serious injury, such as a Monteggia fracture-dislocation, may need to be immobilized for 6 to 10 weeks.
Surgical Treatment
Surgery to align the bones and secure them in place may be required if:
- The skin is broken
- The fracture is unstable — the ends of the broken bones will not stay lined up
- Bone segments have been displaced
- The bones cannot be aligned properly through manipulation alone
- The bones have already begun to heal at an angle or in an improper position
After the bones are aligned, the physician may use pins, metal implants, or a cast to hold them in place until they have healed.
Long-Term Outcome
When the cast is removed, the wrist joint and elbow joint may be stiff for 2 to 3 weeks. This stiffness will go away without the need for physical therapy.
The forearm bones may temporarily be weaker due to the immobilization in the cast. Children should avoid playground structures, such as monkey bars, for 3 to 4 weeks after the cast is removed, in order to allow the bone to safely regain its normal strength.
If the fracture disrupts the growth plate at the end of the bone, your doctor will probably want to watch it carefully for several years to ensure that growth proceeds normally.

 Diagnosis and treatment
Diagnosis and treatment