What are nerves?
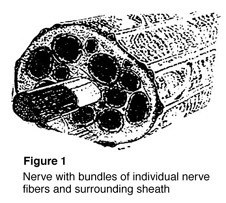 Nerves are the “electrical wiring” system in all people that carry messages from the brain to the rest of the body. A nerve is like an electrical cable wrapped in insulation. A ring of tissue forms a cover to protect the nerve, just like the insulation surrounding an electrical cable (Figure 1).
Nerves are the “electrical wiring” system in all people that carry messages from the brain to the rest of the body. A nerve is like an electrical cable wrapped in insulation. A ring of tissue forms a cover to protect the nerve, just like the insulation surrounding an electrical cable (Figure 1).
Nerves serve as the “wires” of the body that carry information to and from the brain. Motor nerves carry messages from the brain to muscles to make the body move. Sensory nerves carry messages to the brain from different parts of the body to signal pain, pressure, and temperature. While the axon (nerve fiber) carries only one type of message, either motor or sensory, most nerves in the body are made up of both.
What happens when a nerve is injured?
Nerves are fragile and can be damaged by pressure, stretching, or cutting. Injury to a nerve can stop signals to and from the brain causing muscles not to work properly, and you may lose feeling in the injured area. When a nerve is cut, both the nerve and the insulation are broken. Pressure or stretching injuries can cause the fibers carrying the information to break and stop the nerve from working, without damaging the cover.
When nerve fibers are cut, the end of the fiber farthest from the brain dies, while the insulation stays healthy. The end that is closest to the brain does not die, and after some time may begin to heal. If the insulation was not cut, new fibers may grow down the empty cover of the tissue until reaching a muscle or sensory receptor.
If both the nerve and insulation have been cut and the nerve is not fixed, the growing nerve fibers may grow into a ball at the end of the cut, forming a nerve scar or neuroma. A neuroma can be painful and cause an electrical feeling when touched.
How is it treated?
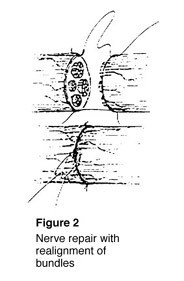 To fix a cut nerve, the insulation around both ends of the nerve are sewn together. The goal in fixing the nerve is to save the cover so that new fibers may heal and work again (Figure 2). If a wound is dirty or crushed, your physician may wait to fix the nerve until the skin has healed.
To fix a cut nerve, the insulation around both ends of the nerve are sewn together. The goal in fixing the nerve is to save the cover so that new fibers may heal and work again (Figure 2). If a wound is dirty or crushed, your physician may wait to fix the nerve until the skin has healed.
If there is a space between the ends of the nerve, the doctor may need to take a piece of nerve (nerve graft) from another part of the body to fix the injured nerve. This may cause permanent loss of feeling in the area where the nerve graft was taken.
Once the nerve cover is fixed, the nerve generally begins to heal three or four weeks after the injury. Nerves usually grow one inch every month depending on the patient’s age and other factors. This means that with an injury to a nerve in the arm above the fingertips, it may take up to a year before feeling returns to the fingertips. The feeling of pins and needles in the fingertips is common during the recovery process. While this can be uncomfortable, it usually passes and is a sign of recovery.
What is my role in recovery and what kind of results can I expect? The patient must do several things to keep up muscle activity and feeling while waiting for the nerve to heal. Your doctor may recommend therapy to keep joints flexible.
If the joints become stiff, they will not work even after muscles begin to work again. When a sensory nerve has been injured, the patient must be extra careful not to burn or cut fingers since there is no feeling in the affected area.
After the nerve has recovered, the brain gets “lazy,” and a procedure called sensory re-education may be needed to improve feeling to the hand or finger. Your doctor will recommend the appropriate therapy based on the nature of your injury.
Factors that may affect results after nerve repair include age, the type of wound and nerve, and location of the injury. While nerve injuries may create lasting problems for the patient, care by a physician and proper therapy help two out of three patients return to more normal use.