Description
The hand and wrist have multiple small joints that work together to produce motion. This gives you the fine motion needed to thread a needle or tie a shoelace. When the joints become affected with arthritis, activities of daily living can be difficult. Arthritis can occur in multiple areas of the hand and wrist. It can have multiple causes.
All arthritic joints lose cartilage, which works as nature’s “shock absorber.” Cartilage provides a smooth gliding surface for the joint. When the cartilage becomes worn or damaged, or is lost due to disease or trauma, the joint no longer has a painless, mobile area of motion.
The body attempts to make up for the lost cartilage. It produces fluid in the joint lining (synovium), which tries to act like a cushion, like water in a waterbed. But it also causes the joint to swell. This restricts motion. The swelling causes stretching of the joint covering (capsule), which causes pain.
Over time, if the arthritis is not treated, the bones that make up the joint can lose their normal shape. This causes more pain and further limits motion.
Risk Factors/Prevention
It is estimated that one out of every five people living in the United States has at least one joint with signs or symptoms of arthritis. About half of arthritis sufferers are under age 50. Arthritis is the leading cause of disability in the United States. It typically occurs from either disease or trauma. The exact number of people with arthritis in the hand and wrist is not known.
When arthritis occurs due to disease, the onset of symptoms is gradual and the cartilage decreases slowly. The two most common forms of arthritis from disease are osteoarthritis and rheumatoid arthritis. Osteoarthritis is much more common and generally affects older people.
It appears in a predictable pattern in certain joints. Rheumatoid arthritis has other system-wide symptoms and may be passed from parent to child (genetically).
When arthritis is due to trauma, the cartilage is damaged. People of any age can be affected. Fractures–particularly those that damage the joint surface–and dislocations are the most common injuries that lead to arthritis (see Figure 1). An injured joint is about seven times more likely to become arthritic, even if the injury is properly treated.
Arthritis does not have to result in a painful or sedentary life. It is important to seek help early so that treatment can begin and you can return to doing what matters most to you.
Diagnosis
A doctor can diagnose arthritis of the hand by examining you and taking X-rays. Specialized studies such as MRI (magnetic resonance imaging) scans are usually not needed. Sometimes a bone scan is helpful (see Figure 2).
A bone scan may help the doctor diagnose arthritis when it is in an early stage, even if X-rays look normal. Arthroscopy is another way to look at the joint by direct inspection. During an arthroscopic procedure, the surgeon inserts a small camera into the joint to look inside.
It provides the clearest picture of the joint without having to make a large incision. However, this is an invasive procedure and should not be used as a routine diagnostic tool (see Figure 3).
Symptoms
Early symptoms of arthritis of the hand include joint pain that may feel “dull,” or a “burning” sensation. The pain often occurs after periods of increased joint use, such as heavy gripping or grasping. The pain may not be present immediately, but may show up hours later or even the following day.
Morning pain and stiffness are typical. As the cartilage wears away and there is less material to provide shock absorption, the symptoms occur even with less use. In advanced disease, the joint pain may wake you up at night.
When the affected joint is subject to greater stress than it can bear, it may swell in an attempt prevent further joint use. Your pain might be made worse with use and relieved by rest. Many people with arthritis complain of increased joint pain with rainy weather. Activities that once were easy, such as opening a jar or starting the car, become difficult due to pain.
To prevent pain at the arthritic joint, you might adapt the way you use your hand. In patients with advanced thumb base arthritis, the neighboring joints may become more mobile than normal (see Figure 4).
The arthritic joint may feel warm to touch. This is due to the body’s inflammatory response. There may be a sensation of grating or grinding in the affected joint (crepitation). This is caused by damaged cartilage surfaces rubbing against one another. If arthritis is due to damaged ligaments, the support structures of the joint may be unstable or “loose.”
In advanced cases, the joint may appear larger than normal (hypertrophic). This is usually due to a combination of bone changes, loss of cartilage and joint swelling.
When arthritis affects the end joints of the fingers (DIP joints), small cysts (mucous cysts) may develop (see Figure 5). The cysts may then cause ridging or dents in the nail plate of the affected finger.
Treatment Options: Nonsurgical
Treatment options for arthritis of the hand and wrist include medication, splinting, injections and surgery. Treatment depends on many factors:
- How far the arthritis has progressed
- How many joints are involved
- Your age, activity level and other medical conditions
- If the dominant or non-dominant hand is affected
Your personal goals, home support structure, and ability to understand the treatment and comply with a therapy program
Medications: Medications treat symptoms but cannot restore joint cartilage or reverse joint damage. The most common medications for arthritis are anti-inflammatories, which stop the body from producing chemicals that cause joint swelling and pain.
Examples of anti-inflammatory drugs include over-the-counter medications such as Tylenol® and Advil® and prescription drugs such as Celebrex®. Glucosamine and chondroitin are widely advertised “neutraceuticals.”
Neutraceuticals are not drugs. Rather, they are compounds that are the “building blocks” of cartilage. They were originally used by veterinarians to treat arthritic hips in dogs. However, neutraceuticals have not yet been studied as a treatment of hand and wrist arthritis.
Injections: When first-line treatment with anti-inflammatory medication is not appropriate, injections may be used. These typically contain a long-acting anesthetic, similar to novacaine but longer lasting, and a steroid that can provide pain relief for weeks to months.
The injections can be repeated, but only a limited number of times, due to possible side effects, such as lightening of the skin, weakening of the tendons and ligaments and infection.
Splinting: Injections are usually combined with splinting of the affected joint. The splint helps support the affected joint to ease the stress placed on it by activities. Splints are typically worn during periods when the joints hurt.
They should be small enough to allow functional use of the hand when they are worn. Wearing the splint for too long can lead to muscle wasting (atrophy). Muscles can assist in stabilizing injured joints, so atrophy should be prevented.
Treatment Options: Surgical
If non-operative treatment fails to give you relief, surgery is usually discussed. There are many surgical options. The option chosen should be one that has a reasonable chance of providing long-term pain relief and return to function. It should be tailored to your individual needs. It is important that the treating physician is well versed in current surgical techniques. If there is any way the joint can be preserved or reconstructed, this option is usually chosen.
When the damage has progressed to a point that the surfaces will no longer work, a joint replacement or fusion (arthrodesis) is performed (see Figure 6). Joint replacements attempt to provide pain relief and functional joint motion. Joint fusions provide pain relief but stop joint motion. The fused joint no longer moves; the damaged joint surfaces are gone, so they cannot cause symptoms.
As with hip and knee replacements, there have been significant improvements in joint replacements in the hand and wrist. The replacement joints are made of materials similar to those used in weight-bearing joints, such as ceramics or long wearing metal and plastic parts (see Figure 7). The goal is to improve the function and longevity of the replaced joint. Most of the major joints of the hand and wrist can be replaced.
A surgeon often needs additional training to perform the surgery. As with any evolving technology, the long-term results of the hand or wrist joint replacements are not yet known. Early results have been promising. Talk with your doctor to find out if these implants are right for you.
After any type of joint reconstruction surgery, there is a period of recovery. Often, you will be referred to a trained hand therapist, who can help you maximize your recovery. You may need to use a postoperative splint or cast for awhile after surgery. This helps protect the hand while it heals.
During this postoperative period, you may need to modify activities to let the joint reconstruction heal properly. Typically, pain medication you take by mouth is also used to reduce discomfort.
It is important to discuss your pain with your doctor so it can be adequately treated. Length of recovery time varies widely and depends on the extent of the surgery performed and multiple individual factors. However, people usually can return to most if not all of their desired activities in about three months after most major joint reconstructions.
Research on the Horizon/What’s New?
Increasingly, doctors are focusing on how to preserve the damaged joint. This includes getting an earlier diagnosis and repairing joint components before the entire surface becomes damaged. Arthroscopy of the small joints of the hand and wrist is now possible because the equipment has been downsized.
There have been encouraging results in cartilage repair and replacement in the larger joints such as the knee, and some of these techniques have been applied to the smaller joints of the hand and arm. In addition, stem cell research may be an option to regenerate damaged joint surfaces.
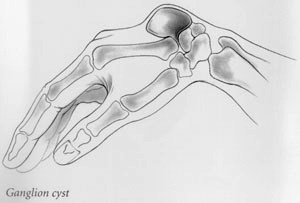 Ganglion cysts are the most common mass or lump in the hand. They are most common on the back of the wrist. These non-cancerous, fluid-filled cysts arise from the ligaments, joint linings, or tendon sheaths when they are irritated or inflamed.
Ganglion cysts are the most common mass or lump in the hand. They are most common on the back of the wrist. These non-cancerous, fluid-filled cysts arise from the ligaments, joint linings, or tendon sheaths when they are irritated or inflamed.  Common symptoms of carpal tunnel syndrome are numbness and tingling in the hand, especially at night; pain with prolonged gripping such as holding a steering wheel; or clumsiness in handling objects. Sometimes the pain can go all the way up to the shoulder.
Common symptoms of carpal tunnel syndrome are numbness and tingling in the hand, especially at night; pain with prolonged gripping such as holding a steering wheel; or clumsiness in handling objects. Sometimes the pain can go all the way up to the shoulder.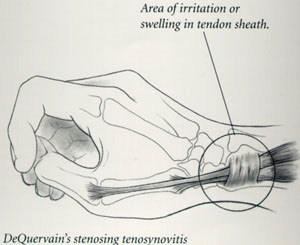 DeQuervain’s stenosing tenosynovitis is an irritation and swelling of the sheath or tunnel which surrounds the thumb tendons as they pass from the wrist to the thumb. Pain when grasping or pinching and tenderness over the tunnel are the most common symptoms.
DeQuervain’s stenosing tenosynovitis is an irritation and swelling of the sheath or tunnel which surrounds the thumb tendons as they pass from the wrist to the thumb. Pain when grasping or pinching and tenderness over the tunnel are the most common symptoms. 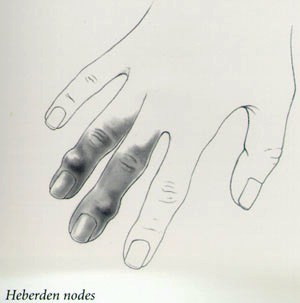 Wear and tear arthritis is very common at the base of the thumb. Pain localized to the base of the thumb, particularly with use, is a very common early symptom.
Wear and tear arthritis is very common at the base of the thumb. Pain localized to the base of the thumb, particularly with use, is a very common early symptom.  Dupuytren’s contracture is a hereditary thickening of the tough tissue called fascia that lies just below the skin of your palm.
Dupuytren’s contracture is a hereditary thickening of the tough tissue called fascia that lies just below the skin of your palm. 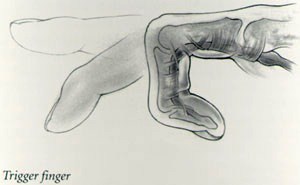 Trigger finger is an irritation of the digital sheath which surrounds the flexor tendons. When the tendon sheath becomes thickened or swollen it pinches the tendon and prevents it from gliding smoothly.
Trigger finger is an irritation of the digital sheath which surrounds the flexor tendons. When the tendon sheath becomes thickened or swollen it pinches the tendon and prevents it from gliding smoothly. 
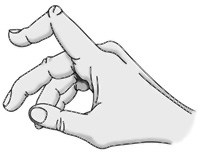 Boutonnière deformity is an injury to the tendons in your fingers that usually prevents the finger from fully straightening. The result is that the middle joint of the injured finger bends down, while the fingertip bends back. This is the characteristic shape of a boutonnière deformity. Unless this injury is treated promptly, the deformity may progress, resulting in permanent deformity and impaired functioning.
Boutonnière deformity is an injury to the tendons in your fingers that usually prevents the finger from fully straightening. The result is that the middle joint of the injured finger bends down, while the fingertip bends back. This is the characteristic shape of a boutonnière deformity. Unless this injury is treated promptly, the deformity may progress, resulting in permanent deformity and impaired functioning.