from orthoinfo.aaos.org
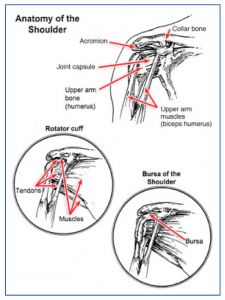
It is made up of three bones: the scapula (shoulder blade), the clavicle (collarbone) and the humerus (upper arm bone). The true shoulder joint is where the shoulder blade meets the upper arm bone.
A second joint exists where the collarbone meets the shoulder blade on the top and front of the shoulder and is called the AC or acromioclavicular joint. When people refer to a shoulder separation, it is really the AC joint that has been injured, not the true ball and socket (glenohumeral) joint of the shoulder. A third joint exists where the shoulder blade sits on the back of the ribcage called the scapulothoracic joint.
The shoulder joint is unique in that it can move in almost every direction, unlike the knee that just straightens and bends. The large ball on the relatively flat socket is what allows the shoulder such unrestricted motion.
What keeps the humeral head (the ball) on the flat surface of the glenoid (socket) is the muscles, tendons, and ligaments that surround the head plus a lip of cartilage (labrum) that surrounds and extends the socket to help contain the head.
The rotator cuff is a group of 4 muscles that converge on the outside of the shoulder to help elevate and rotate the arm. The tendinous attachment of these tendons to the upper arm bone is called the rotator cuff. The long head of the biceps tendon also runs over the top of the shoulder and attaches to the upper part of the socket through the upper labrum.
Between the top of the shoulder blade (the acromion) and the rotator cuff and biceps tendons is a large fluid filled sack called the bursa. It is normally quite thin and helps allow these tissues to slide under the acromion without rubbing or abrading.

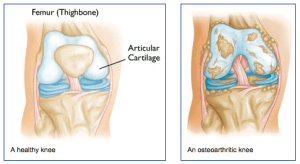 What is arthritis of the knee?
What is arthritis of the knee? The physician’s work-up will start with a careful history and exam. A history of prior injury, pain, stiffness and swelling may suggest arthritis. The exam often shows some swelling and decreased range of motion. Sometimes, patients develop deformities if one side of the knee wears out more than the other side.
The physician’s work-up will start with a careful history and exam. A history of prior injury, pain, stiffness and swelling may suggest arthritis. The exam often shows some swelling and decreased range of motion. Sometimes, patients develop deformities if one side of the knee wears out more than the other side. 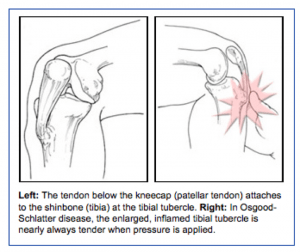 Diagnosis
Diagnosis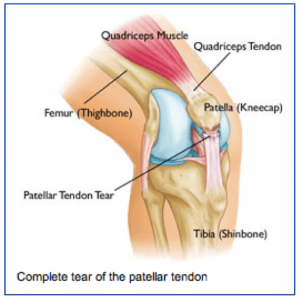 Anatomy
Anatomy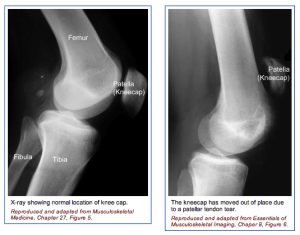 The physician’s work-up will start with a careful history and exam. The physician can often feel the defect in the quadriceps tendon and can appreciate the weakness on trying to straighten out the knee against resistance.
The physician’s work-up will start with a careful history and exam. The physician can often feel the defect in the quadriceps tendon and can appreciate the weakness on trying to straighten out the knee against resistance.