 Description
Description
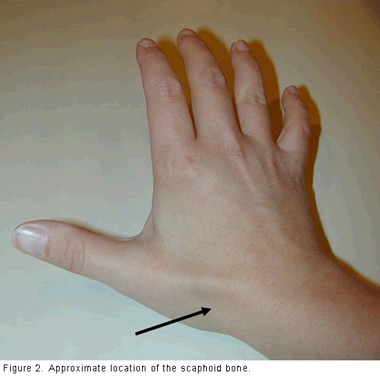
The scaphoid is one of the small bones in the wrist (carpal bones), and the one that is most likely to break. The scaphoid is located on the thumb side of the wrist, in the area where the wrist bends (see Figure 1).When you hold your thumb in a “hitch hiking” position, the scaphoid is at the base of the depression made by your thumb tendons. Pain or tenderness in this area can be a sign that the scaphoid is injured (see Figure 2).
A fracture of the scaphoid usually happens when you fall on an outstretched hand, with your weight landing on the palm. The end of the forearm bone (radius) may also break in this type of fall, depending on the position of the hand when you land. Pain and swelling in the wrist will usually cause a person with a scaphoid fracture to see a doctor. If the wrist is not deformed, however, you might not know that you have a broken bone–people sometimes think they have just sprained the wrist.
It is important to see your doctor if you have pain on the thumb side of the wrist that starts after a fall or accident and does not go away within a few days. The doctor will probably order X-rays to look at the bone.
 Sometimes, a broken scaphoid does not show up on an X-ray right away. When this is the case, the doctor may put your wrist in a splint and wait to take a new X-ray in a week or two, when the fracture may become visible. Keep the splint on and do not do any heavy lifting during the waiting time.
Sometimes, a broken scaphoid does not show up on an X-ray right away. When this is the case, the doctor may put your wrist in a splint and wait to take a new X-ray in a week or two, when the fracture may become visible. Keep the splint on and do not do any heavy lifting during the waiting time.
Your doctor might also recommend an MRI (magnetic resonance image) to see the bones and soft tissues. An MRI can sometimes show a fracture of the scaphoid before it can be seen on an X-ray.
Risk Factors/Prevention
Fractures of the scaphoid occur in people of all ages, including children. The injury often happens during sports activities or a motor vehicle accident. Men aged 20 to 30 years are most often affected.
There are no specific risks or diseases that increase the chance of having a scaphoid fracture. Some studies have shown that use of wrist guards during activities like inline skating and snowboarding can decrease the chance of breaking a bone around the wrist.
Symptoms
Scaphoid fractures usually cause pain in the base of the thumb, with swelling in the same area. You may have severe pain when you move your thumb or wrist or grip anything. Other times, the pain is not so bad, and you may mistakenly think that you just sprained your wrist.
Treatment Options
Treatment of scaphoid fractures depends on the location of the break in the bone. Sometimes, the scaphoid is broken at the end near the thumb. This part of the bone has a good blood supply. Scaphoid fractures in this location usually heal in a matter of weeks with proper protection. The time frame to healing is best determined by X-rays or other imaging studies such as a CT scan, which confirm that the bone has healed. Most fractures here heal well when they are placed in a cast. The cast will usually be below the elbow. It may or may not include the thumb.
More commonly, the scaphoid is broken in the middle (waist) or at the part closer to the forearm (proximal pole). This part of the scaphoid does not have a very good blood supply, so it is more difficult to heal. If your orthopaedist recommends that your scaphoid fracture be treated in a cast, it will probably include the thumb. Sometimes the cast will extend to above your elbow and may also include your index finger.
Treatment Options: Surgical
Often, when the scaphoid is broken at the waist or proximal pole, an orthopaedist will recommend surgery using a screw or wire to stabilize the scaphoid from the inside while the bone heals (see Figure 3). Depending on what part of the scaphoid is broken, the incision will be on the front or the back of the wrist (see Figure 4). Sometimes the screw or wire is placed with just a small incision.
Other times a bigger incision is needed to ensure that the pieces of the scaphoid are put back together well. Usually your wrist will be placed in a cast after the surgery, sometimes for a few months. Even with surgery, fractures in this area can take a long time to heal, and it is possible that a nonunion or avascular necrosis will occur.
If the scaphoid does not heal, either with or without initial surgery, your orthopaedist may recommend an operation to add bone graft to the scaphoid to help it heal. The surgeon may order an MRI or CT (computed tomography) scan to show more detail about position of the broken pieces of the scaphoid, to help plan the operation. Many kinds of bone graft can be used–your surgeon will discuss which one is best for you. Bone graft may be taken from a bone in the forearm or the pelvis or it may be manufactured. Sometimes a special kind of bone graft with its own blood supply (vascularized graft) may be used.

Nonunions, Avascular Necrosis and Arthritis
A bone that fails to heal is called a nonunion; this happens more often in scaphoid fractures than in fractures of many other bones. To heal properly, the bones need blood to carry oxygen and nutrients to the site of the fracture. The scaphoid bone has a poor blood supply. When the scaphoid is broken, especially when broken parts have moved apart (displaced), the blood supply may be disrupted.
Sometimes, the blood supply to one of the broken pieces is so poor that the piece does not get enough nutrients and the cells in the piece die. This is called avascular necrosis. Both nonunion and avascular necrosis of the scaphoid can lead to arthritis of the wrist.
Symptoms of arthritis in the wrist that results from scaphoid nonunion or avascular necrosis include:
- Aching in the wrist
- Decreased range of motion of the wrist
- Pain with activities such as lifting or gripping
If X-rays show arthritis in the wrist because of an old break in the scaphoid, treatment focuses on improving the symptoms of arthritis. At first, this may include taking anti-inflammatory medicine (such as ibuprofen) and wearing a splint when the wrist is painful. Sometimes the doctor may give you a steroid injection into the wrist to help to lessen wrist pain. If this does not work, the doctor may recommend surgery. Many types of operations can be performed for wrist arthritis. Your surgeon will discuss the risks and benefits of the surgery that will be most helpful to you.
Rehabilitation
You will have to wear a cast or splint while the scaphoid fracture is healing, perhaps for as long as six months. Your doctor will give you specific limitations.
Most commonly, you should:
- Avoid heavy lifting, carrying, pushing, pulling or throwing with the injured arm
- Not participate in contact sports
- Not climb ladders or trees
- Avoid activities with a risk of falling onto your hand (for example, inline skating, jumping on a trampoline.
Some people have stiffness in the wrist after scaphoid fractures; this is more common when a cast was needed for a long time and when surgery was done through a long incision. Your orthopaedist may recommend hand therapy to help regain the motion and strength in your wrist. Even with therapy, some people do not recover the same motion and strength in their wrist that they had before the injury.
Research on the Horizon/What’s New?
Some orthopaedists are placing a screw in the scaphoid through a very small incision–about one-fourth to one-half inch. This may decrease the chances of long-term stiffness in the wrist by decreasing the time that a full-time cast needs to be worn. This is done using a special X-ray machine during surgery to help guide the placement of the screw. Some surgeons use this method even when the broken pieces of the scaphoid are out of place. By looking directly at the scaphoid with a tiny camera (an arthroscope), the surgeon can tell when the broken pieces are lined up.
There is a lot of research being done about the best way to treat fractures of the scaphoid that are not healing well. Some of this research looks at different types of bone graft, including vascularized grafts. New types of manufactured bone graft with special bone cell components to increase healing are being tried to help bones that are not healing.

 Description
Description 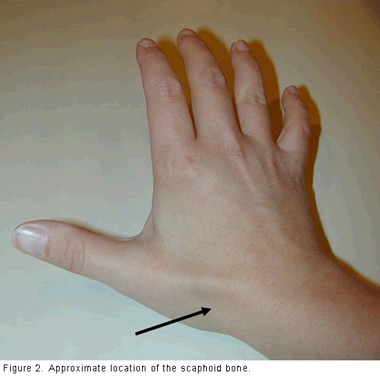 Sometimes, a broken scaphoid does not show up on an X-ray right away. When this is the case, the doctor may put your wrist in a splint and wait to take a new X-ray in a week or two, when the fracture may become visible. Keep the splint on and do not do any heavy lifting during the waiting time.
Sometimes, a broken scaphoid does not show up on an X-ray right away. When this is the case, the doctor may put your wrist in a splint and wait to take a new X-ray in a week or two, when the fracture may become visible. Keep the splint on and do not do any heavy lifting during the waiting time.