Perhaps it starts as a very low grade aching in the wrist, barely enough to get your attention. Then the pain becomes more frequent and persistent. As you roll your wrist around in circles trying to figure out the cause, you notice a small bump on the back of the wrist. Of course, your next move is to do the same with the opposite wrist to see if it’s present on both sides. Nothing. No bump. Time to see the doctor.
Finding a lump on your body that you know was not there previously is generally concerning. Most bumps on the hand are not cancerous, but are important to have checked out promptly by a hand surgeon. In this case, a common cause is a ganglion cyst, a small mass that can develop around the joints of the wrist and hand. Ganglion cysts are benign, fluid filled sacs that may or may not cause pain in the affected area. They are the most common form of mass found in the hand and are generally found in younger individuals between the ages of 15-40.
The most common location is on the back of the wrist, but they may also be found on the palm side of the wrist or at the base of the fingers. The cause is not known, but often times there is a correlation between their development and chronic, mechanical stress in the wrist or hand. Athletes that have repetitive stress on the wrist and hand such as gymnasts have been found to have a higher incidence of these cysts developing.
These cysts may also develop at the most distal joint of the finger. This type of cyst, called a mucous cyst, is associated with wear and tear in the finger joints and is more common with age.
In my practice, ganglion cysts are a relatively common occurrence. The diagnosis is generally straightforward, usually requiring only a physical exam and occasionally an X-ray. The size and shape of the lump, along with its location, are generally sufficient to make an accurate diagnosis, but I sometimes will order an MRI if there is any uncertainty.
In most cases, these cysts are harmless and the treatment can be as simple as periodic observation for any changes that impact movement or function of the wrist or hand. Sometimes, the ganglion can disappear by itself. In cases where the cyst causes pain or becomes an impediment to movement and function, there are more aggressive treatments available. Often, the cysts are simply persistent and unsightly, requiring removal.
First of all, if you have been surfing the internet you may have read that ganglion cysts used to be called “Bible cysts” because in times past, a treatment was to slam a bible or other heavy book over the cyst, causing it to burst. DON’T DO IT. It is not effective and you could end up with a broken bone in your hand. It is just not worth trying.
Aspiration is usually the first treatment method used to reduce a ganglion. A small needle is inserted into the cyst and the fluid is drained. This produces an immediate reduction in the size of the lump. This is performed in the office setting, and there are no significant restrictions following the procedure. The downside is that the ganglion cyst may return in at least 50% of patients. This is because the root and capsule of the cyst is left intact. An analogy would be to think of deflating a balloon. With fluid production, the balloon can simply re-inflate. Even though the permanent success of aspiration is relatively low, given the ease and simplicity of the aspiration procedure, it is still often worth a try.
Should the cyst return following needle aspiration, surgery may be required that removes the capsule and root completely. This is an outpatient surgical procedure performed under a light anesthesia – usually a combination of a local anesthetic and a sedating medicine administered by the anesthesiologist. The ganglion plus a small amount of the joint capsule or tendon sheath from which the cyst stems is removed. Following surgery, the hand will be splinted for a short duration, and the patient will be able to return to normal activities within 2-4 weeks. Physical or occupational therapy is usually not needed, but a referral may be made in instances where a patient has significant stiffness in the hand or wrist joints. Although there is a small risk of the cyst returning, my patients enjoy a high success rate, with over 90% of all excisions being permanent.
It is important to have any persistent mass checked out by a physician. He or she can perform the appropriate physical exam and testing to confirm the diagnosis and refer you to the appropriate specialist if necessary. If you should have any questions regarding this or any other conditions of the hand, wrist or elbow, please feel free to contact our office at (206) 633-8100, ext. 18133 to schedule a consultation.

 We see many patients who have lumps and bumps in their hand that are painful, growing, affect function, and are often worry some for the patient due to the concern for cancer. If you are concerned about a hand tumor, wrist mass, or finger cyst, you should schedule a consultation to put your mind at ease with a diagnosis and to discuss treatments available.
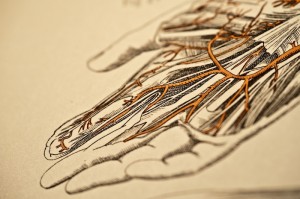
We see many patients who have lumps and bumps in their hand that are painful, growing, affect function, and are often worry some for the patient due to the concern for cancer. If you are concerned about a hand tumor, wrist mass, or finger cyst, you should schedule a consultation to put your mind at ease with a diagnosis and to discuss treatments available. 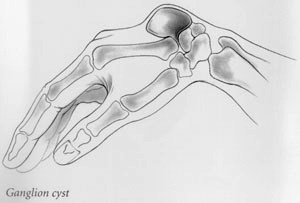 Ganglion cysts are the most common mass or lump in the hand. They are most common on the back of the wrist. These non-cancerous, fluid-filled cysts arise from the ligaments, joint linings, or tendon sheaths when they are irritated or inflamed.
Ganglion cysts are the most common mass or lump in the hand. They are most common on the back of the wrist. These non-cancerous, fluid-filled cysts arise from the ligaments, joint linings, or tendon sheaths when they are irritated or inflamed.  Common symptoms of carpal tunnel syndrome are numbness and tingling in the hand, especially at night; pain with prolonged gripping such as holding a steering wheel; or clumsiness in handling objects. Sometimes the pain can go all the way up to the shoulder.
Common symptoms of carpal tunnel syndrome are numbness and tingling in the hand, especially at night; pain with prolonged gripping such as holding a steering wheel; or clumsiness in handling objects. Sometimes the pain can go all the way up to the shoulder.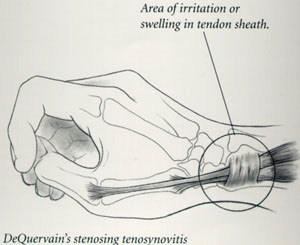 DeQuervain’s stenosing tenosynovitis is an irritation and swelling of the sheath or tunnel which surrounds the thumb tendons as they pass from the wrist to the thumb. Pain when grasping or pinching and tenderness over the tunnel are the most common symptoms.
DeQuervain’s stenosing tenosynovitis is an irritation and swelling of the sheath or tunnel which surrounds the thumb tendons as they pass from the wrist to the thumb. Pain when grasping or pinching and tenderness over the tunnel are the most common symptoms. 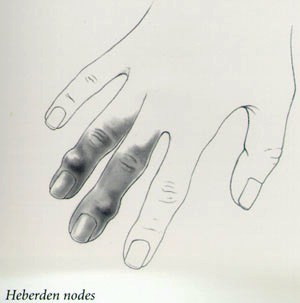 Wear and tear arthritis is very common at the base of the thumb. Pain localized to the base of the thumb, particularly with use, is a very common early symptom.
Wear and tear arthritis is very common at the base of the thumb. Pain localized to the base of the thumb, particularly with use, is a very common early symptom.  Dupuytren’s contracture is a hereditary thickening of the tough tissue called fascia that lies just below the skin of your palm.
Dupuytren’s contracture is a hereditary thickening of the tough tissue called fascia that lies just below the skin of your palm. 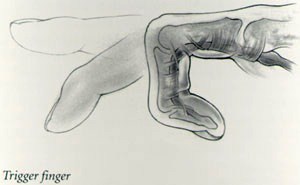 Trigger finger is an irritation of the digital sheath which surrounds the flexor tendons. When the tendon sheath becomes thickened or swollen it pinches the tendon and prevents it from gliding smoothly.
Trigger finger is an irritation of the digital sheath which surrounds the flexor tendons. When the tendon sheath becomes thickened or swollen it pinches the tendon and prevents it from gliding smoothly.