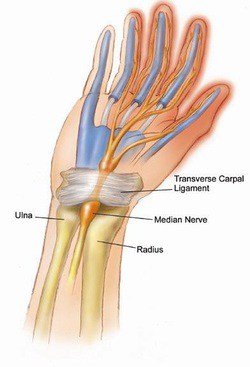
Other common names: Distal Radius Fracture, Fracture of the end of the Radius, Broken Wrist, Wrist FractureWhat is a Broken Wrist?Though there are 10 bones that make up the wrist, and each bone has the potential to fracture (medical term for broken bone), by far the most common broken bone in the wrist is a fracture of the end of the radius bone (Figure 1). Other common injuries include a wrist sprain, scaphoid fracture, Ulna fracture, fracture of the triquetrum.
Typically, a patient sustains a broken wrist from one of two scenarios; one is that they were in an accident, or fell with such force on their hand that the otherwise normal wrist crushed under significant forces. The second scenario involves one with less than ideal bone density who falls on an outstretched hand in a way that causes the bone to break. The difference between the two is the difference in the quality of the bone and the amount of force required to break the bone. The distinction between the two mechanisms is significant as the patient with higher quality bone often has multiple injuries due to the significant force of the injury, and in the patient with poorer bone quality, a thorough bone quality investigation should be considered.
How are Fractures to the end of the Radius evaluated?
X-rays and a physical exam can usually give the information needed to evaluate a distal radius fracture. Occasionally, further imaging such as a CT or MRI may be considered, but this is rare. In addition to the bone, there is certainly injury to the surrounding soft structures such as tendons, ligaments, muscles and nerves which will affect your outcome.
How is my broken wrist going to be treated? Do I need surgery?
Many factors go into deciding the best treatment for your wrist fracture, but typically I choose the treatment regimen which will allow the best recovery potential, both in the short term and in the long term. This usually initially involves an attempt at manipulating the fracture into the most ideal healing position and holding that position with a splint or cast. If the wrist fracture falls into an unacceptable position for healing despite maximal non-operative care, then surgical intervention is considered. With experience, training and careful review of current research, I can often predict which fractures can be treated without surgery and which ones will need further surgical stabilization.
How long is the recovery from my broken wrist?
Most patients, regardless of the type of break, have very good long term results. Most fractures treated without surgery will require 6 weeks in a cast, and another 6 weeks to regain most of the strength that was lost. Distal Radius fractures which require surgical stabilization often only need 2 weeks of splinting, followed by 4 weeks of exercise to regain range of motion and another 6 weeks to regain strength. Most patients are able to do most activities by three months after the injury, but individual circumstances certainly vary.

 What is it?
What is it?