Arthroscopy (ar-THROS-ka-pea) is an outpatient surgical procedure used by orthopaedic surgeons to diagnose and treat problems inside a joint. The surgeon makes small incisions, less than half an inch long, and inserts a pencil-sized instrument called an arthroscope. The arthroscope contains a small lens, a miniature camera and a lighting system. This projects three-dimensional images of the joint on a television monitor, enabling the surgeon to look directly inside the joint and identify the trouble. Tiny probes, forceps, knives and shavers can then be used to correct many problems at the same time.
Ulnar Tunnel Syndrome
Most people are familiar with carpal tunnel syndrome, which can cause numbness and tingling in the hand. A similar condition, called ulnar tunnel syndrome, can cause numbness and tingling that is confined to your little finger and the outside of your ring finger. Unlike carpal tunnel syndrome, however, ulnar tunnel syndrome is not usually caused by repetitive motions.
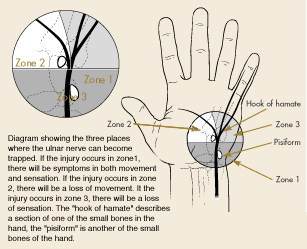
The ulnar nerve is one of three major nerves that provide sensation and motor function to the hand. It runs down the inside of your forearm to the heel of your hand. Then it branches out across the palm and into the little and ring fingers. Excessive pressure on this nerve can result in a loss of feeling and/or muscle weakness in the hand.
Signs and symptoms
You may or may not have pain in your hand, but you will probably experience weakness and increasing numbness, particularly on the little finger side of the hand. You may experience sensory or motor changes or both, depending on the location of the pressure point. Symptoms develop gradually and can lead to difficulties in opening jars, holding objects, or coordinating your fingers while typing or playing a musical instrument.
Diagnosis
Your physician may examine your hand to see if there are any signs of muscle shrinkage (atrophy) or weakness. To test sensory involvement, he or she may tap a finger over the nerve to see if this produces a tingling sensation (Tinel sign). When you spread your fingers apart, the doctor will look for signs of muscle weakness or dry skin in the spaces between your fingers. Your doctor may prescribe a nerve conduction study to see if the nerve is working properly. A computed tomography scan or a magnetic resonance image (MRI) may be useful in identifying whether a cyst or other growth is putting pressure on the nerve. X-rays can show if you’ve fractured a bone that is now pressing on the nerve. The ulnar nerve also passes through a narrow tunnel at the elbow. Pressure at that point can cause similar symptoms in your hand. So your physician may examine that area as well.
Treatment
 Treatment depends on what’s causing the pressure on the nerve. If pressure results from the way you rest your wrist when typing, a change in position or the addition of some padding may help.
Treatment depends on what’s causing the pressure on the nerve. If pressure results from the way you rest your wrist when typing, a change in position or the addition of some padding may help.
Your doctor may prescribe anti-inflammatory medications such as aspirin or ibuprofen to help alleviate your symptoms, and may recommend that you wear a wrist splint for a time. However, most cases of ulnar tunnel syndrome are caused by a growth in the wrist and must be treated with surgery to remove the growth.
An experienced hand surgeon can remove cysts, scar tissue, or other causes of compression on an outpatient basis. Once the pressure point is removed, you’ll notice an improvement in sensation with a decrease in the numbness and tingling. But it will take several months for the nerve to regrow and heal completely. Your surgeon will make recommendations for postoperative rehabilitation and exercises.
Trigger Finger
A trigger finger is a common problem that causes pain and catching. Tendons that help bend the fingers and thumb slide through a snug tunnel. Irritation as the tendons slip into the tunnel can cause the opening of the tunnel to become smaller, or the tendon to thicken so that it can’t easily pass through the tunnel.
As you try to straighten the finger, the tendon becomes momentarily stuck at the mouth of the tunnel then pops as the tendon slips past the tight area. This can cause pain and catching as you try to move the finger. Your doctor can diagnose the problem by talking with you and examining your hand. No X-rays or other testing are usually needed.
Thumb Fractures
The thumb has two finger bones connected to a hand bone. The first finger bone (distal phalange) extends from the tip of the thumb to the knuckle. The second finger bone (proximal phalange) extends from the knuckle to the webbing between the thumb and the first finger. There, it connects with the hand bone (first metacarpal), which extends from the webbing down to the wrist.
Although a break can occur in any of these bones, the most serious breaks happen near the joints, particularly at the base of the thumb near the wrist.
These fractures have specific names, depending on the type of break. The Bennett and Rolando fractures are breaks at the base of the thumb, involving the joint between the thumb metacarpal and a specific wrist bone. Fractures that involve the joints are always more difficult to treat and are at increased risk of an unfavorable outcome.
Scaphoid Fracture
The scaphoid is one of the small bones in the wrist (carpal bones), and the one that is most likely to break. The scaphoid is located on the thumb side of the wrist, in the area where the wrist bends (see Figure 1).When you hold your thumb in a “hitch hiking” position, the scaphoid is at the base of the depression made by your thumb tendons. Pain or tenderness in this area can be a sign that the scaphoid is injured.
