Carpal Tunnel Syndrome
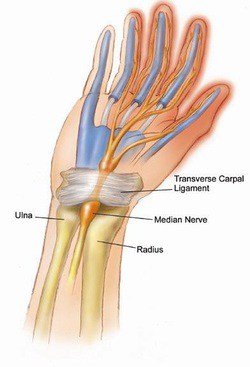
The Carpal Tunnel – The Median Nerve’s Path to the Hand
What is Carpal Tunnel Syndrome?
Carpal tunnel syndrome is a common condition in the adult hand, affecting nearly 3% of the population and is the most common peripheral nerve compression syndrome. The carpal tunnel is a bony passageway in the wrist, housing both the median nerve along with nine wrist flexor tendons.
Due to the nonconforming shape of the tunnel, any increase in the pressure of the tunnel causes compression on the median nerve, thereby decreasing its ability to function properly. The median nerve controls important muscles in the hand, giving sensation to many of the digits.
Carpal tunnel syndrome occurs when the median nerve is compressed as it passes through this tunnel in the hand. When compressed, the median nerve causes numbness, tingling, weakness and pain in the hand and wrist. The pain is often positional, meaning that extreme flexion or extension of the wrist exacerbate the symptoms.
What are the symptoms?
Compression of the median nerve reliably causes numbness in the thumb, index finger, middle finger and half of the ring finger. In addition, if the median nerve is compressed for a critical period of time, the nerve loses its ability to power key muscles of the thumb and hand, causing a loss of strength and dexterity for fine movements.
Other common symptoms include hand pain which is often worse at night or while driving, and a need to shake the hand to allow the hand to “wake up”.
What causes Carpal Tunnel Syndrome?
Contrary to much of the information readily available for patients, it is important to emphasize that the vast majority of patients have no known cause for their carpal tunnel syndrome. While it is tempting to attach blame to repetitive activity such as typing, or blame a particular injury, many well designed objective studies have consistently failed to show any effect of repetitive activity on the development or exacerbation of carpal tunnel syndrome.
The best evidence suggests that some patients likely have a genetic predisposition to the development of carpal tunnel syndrome, despite intuitive interventions such as ergonomic workplace environments or other similar modifications.
Caveat: This is not to say that ergonomic improvements in the way we live and work are not positive improvements. Many significant advances have been made in workplace safety, and certainly in a patient with known carpal tunnel syndrome, minor modifications can be made which can decrease one’s symptoms. However it is important to underscore the fact that though these interventions may help symptomatic management, the lack of such interventions are not the cause of carpal tunnel syndrome.
What are the treatment options?
Treatment usually begins with wrist splints, especially at night, anti-inflammatory medications, and activity modifications. Steroid injections into the carpal tunnel may also provide relief of symptoms, but unfortunately no interventions short of surgery give adequate space for the nerve in the carpal tunnel once there is too much pressure. Ultimately, surgery may be necessary to relieve the pressure on the median nerve in the carpal tunnel.
What is involved in surgery?
Carpal tunnel surgery involves an incision in the base of the palm to gain access to the carpal tunnel. The goal of surgery is to provide more space to for the constricted nerve, which the 30 minute procedure reliably accomplishes. I perform the procedure typically in an outpatient setting and most patients have only a few days of discomfort from the incision are able to use their hand fully by 2 weeks after the sutures are removed. Many patients are able to return to work within 1-3 days, and the dressing stays in place until the sutures are removed.
It is important to note that in severe cases, the nerve has sustained permanent injury from years of compression. Though the surgery reliably relieves pressure on the nerve, sometimes the damage is irreversible and persistent numbness or weakness remain. Interested in learning more about your symptoms? Contact Dr. Scott Ruhlman’s office at 206-633-8100.
