 Anatomy
Anatomy
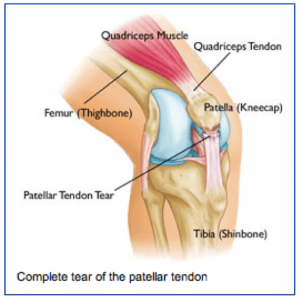
The patellar tendon attaches the lower pole of the kneecap (patella) to the lower leg bone (tibia). The quadriceps muscle attaches to the upper pole of the kneecap and pulls through the kneecap and patellar tendon to allow one to straighten out ones leg or to support ones weight while squatting.
When the patellar tendon is torn, one cannot support their weight when the knee is bent, such as getting up from a chair or going down the stairs.
Injury Mechanism
The patellar tendon is usually injured with a sudden high force across the tendon, such as landing from a jump. The patellar tendon can be injured by a direct blow or a sharp laceration across the tendon.
Symptoms
Patellar tendon injuries present as significant pain across the front of the knee and immediate weakness in supporting ones weight while squatting. Patients usually cannot straighten their knee out fully with a complete tear of the patellar tendon. Rapid swelling occurs. Often, one can feel a gap under their kneecap at the site of the rupture.
Diagnosis
 The physician’s work-up will start with a careful history and exam. The physician can often feel the defect in the patellar tendon and can appreciate the weakness on trying to straighten out the knee against resistance.
The physician’s work-up will start with a careful history and exam. The physician can often feel the defect in the patellar tendon and can appreciate the weakness on trying to straighten out the knee against resistance.
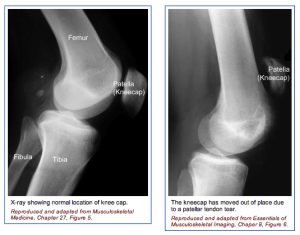
X-rays reveal a very high riding patella, since the pull of the quadriceps is no longer opposed by the tethering effect of an intact patellar tendon.
An MRI scan is often obtained to confirm the diagnosis, especially if the physician is concerned that the injury may be just a partial tear that may be able to heal without surgical repair. Plain x-rays show the bones of the knee, while MRI scans reveal the soft tissues around the knee including the ligaments, menisci, muscles and tendons.
Treatment
Your physician will discuss treatment options with you. Treatment decisions are based on whether the injury is a complete tear or a partial tear. Partial tears may be able to be treated with a brace. The brace is initially locked out completely straight to take all of the pressure off of the injured tendon.
As healing occurs, the hinges are unlocked and motion and strengthening are initiated. With complete tears, surgery is almost always recommended. Surgery involves sewing the two ends of the tendon together with strong suture material. If the tendon has pulled directly off of the bone, drill holes are made into the bone to repair the tendon directly to the bone. Risks and benefits of surgery are discussed thoroughly with the patient.
What to expect after surgery
Patellar tendon surgery is usually performed as an outpatient procedure. Patients are sent home with crutches and a knee brace with the knee fully straightened to protect the repair. Depending on the strength of the repair, patients start gentle range of motion and progressive weight bearing over 6-8 weeks.
Patients are using a stationary bike by 2 months, and an elliptical or stair climber shortly thereafter. Jogging is restricted until 4 months following surgery and full sports activities are not resumed until 6 months after surgery. Most patients can return to full activities, with no restrictions and no bracing at the 6th month point.

 Sports injuries can be divided into two broad categories: repetitive injuries and traumatic injuries. Every sport involves some physical risk in one or both categories. Below you will find some of the more popular sports in the Seattle area along with the major potential risks involved. The following sports are ranked amongst the most popular youth sports in America (Matthew, 2010), or are rising quickly in popularity.
Sports injuries can be divided into two broad categories: repetitive injuries and traumatic injuries. Every sport involves some physical risk in one or both categories. Below you will find some of the more popular sports in the Seattle area along with the major potential risks involved. The following sports are ranked amongst the most popular youth sports in America (Matthew, 2010), or are rising quickly in popularity.