OSS will be closed Thanksgiving, Thursday, November 24th, and the day after Thanksgiving, Friday, November 25th, 2022.
Closed for Thanksgiving Holiday
OSS will be closed Thanksgiving, Thursday, November 25th, and the day after Thanksgiving, Friday, November 26th, 2021.
What is triple arthrodesis?
Arthrodesis
Arthrodesis is a medical term that describes fusion. In a fusion, the bones are locked together by removing the cartilage from the joint surface and creating a “bone bridge” across the joint. A triple arthrodesis is a fusion in the hindfoot (back of the foot) used to treat many types of painful foot deformities. This procedure fuses the joints under the ankle that allow the foot to move from side to side. These joints are the talonavicular, subtalar, and calcaneocuboid.
Surgeons try to avoid fusions, but sometimes pain and deformity are so severe that this procedure offers the best chance of producing a less painful foot with better alignment. Fusions often improve stability and allow for easier standing and walking. The hindfoot fusion is a time-tested, durable procedure.
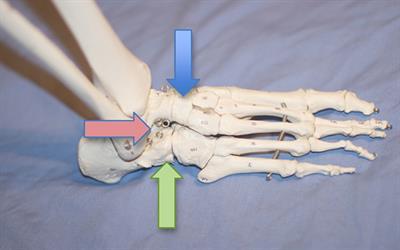
Triple arthrodesis fuses three joints in the back of the foot: the talonavicular (blue arrow), subtalar (red arrow), and calcaneocuboid (green arrow)
Diagnosis
A hindfoot fusion is indicated for severe arthritis, instability, or a deformity that cannot be controlled with non-surgical treatments. Other conditions, such as severe flatfoot, abnormal connections between bones, excessively high arches, and joint instability due to neuromuscular disease, also can indicate the need for a fusion.
Patients who are still growing are not ideal candidates as they may develop additional deformity as they grow. Patients who use tobacco, have an active infection, or have poor healing potential are at higher risk for complications. Non-surgical measures such as bracing and anti-inflammatory medications should be tried first. If another surgical procedure that leaves the joint intact can achieve the same goal, that procedure is preferred over a fusion.
Treatment
In a triple arthrodesis, your foot and ankle orthopedic surgeon makes one incision on each side of the foot, and works in each joint, removing cartilage, roughening bony surfaces, and filling defects. Once all the desired joints have been prepared, they are put into an appropriate position and hardware is placed to stabilize the reconstruction and promote healthy fusion.
Recovery
The rate of healing is variable and is influenced by many factors. In general, the foot is placed into a splint and kept elevated with no weight on it for the first two weeks to minimize swelling and allow for healing of the skin. Stitches may be removed 2-3 weeks after surgery.
Different weight-bearing protocols may be used. After signs of healing are noted, progressive weight bearing is allowed until full weight bearing is reached. This typically takes three months. During this process, the foot may be placed into a cast. Sometimes, a removable boot may be used rather than a cast.
Risks and Complications
All surgeries come with possible complications, including the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Most patients are satisfied with their outcome once they achieve successful fusion. In fact, most feel that the loss of motion is a very acceptable trade-off for pain reduction. In the first two to three weeks, the most likely complication is wound breakdown and/or infection. These are best avoided by not smoking, elevating the foot, avoiding any weight on the foot, and keeping the surgical dressing clean and dry. There also is the risk of the bones not fusing (a non-union). Smoking may place you at increased risk for non-union.
The most common long-term consequence of triple arthrodesis is gradual development of arthritis in other joints of the foot and ankle. These changes can take years or even decades to develop and many never become noticeable to the patient.
FAQs
Will I have stiffness after surgery?
Yes, you can expect some degree of stiffness in your foot as a result of the surgery. You will maintain up-and-down motion, but side-to-side motion will become limited. This will be most noticeable on uneven surfaces but is usually a good trade-off for reasonable pain relief, improved stability and/or deformity correction. Many patients who undergo this surgery have a stiff, painful foot to begin with; after surgery the stiffness may remain but the pain will be relieved.
Will I be able to return to my usual activities?
You can generally expect to return to most activities in life, but the stiffness in side-to-side motion will limit certain activities requiring this motion.
When can I expect to have recovered from a triple arthrodesis?
A significant amount of healing will occur in the first three months. However, it takes about one year for maximum improvement.
Are there side effects to triple arthrodesis?
As one part of the foot is made stiffer, other structures are forced to accept more stress, which increases the chances that they may wear out. This often takes many years or decades to become noticeable.
Will I be able to fit into regular shoes?
Typically patients fit into a shoe after surgery better than before surgery.
When will I be able to bear weight on my foot?
Partial weight bearing typically is allowed once incisions have healed. Full weight bearing generally takes between 2 and 4 months.
What is total ankle replacement?
Total ankle replacement, also known as total ankle arthroplasty, is a surgical procedure that foot and ankle orthopedic surgeons use to treat ankle arthritis. Arthritic changes may be a result of normal wear and tear due to aging or from an injury such as a broken ankle or dislocation. Arthritis eventually leads to loss of cartilage, pain, and/or deformity.
In this procedure, the ankle joint is removed and replaced with an artificial implant made of metal and plastic. The goal of ankle replacement is to provide pain relief while preserving ankle motion so the patient has less pain and better function during activity.
Diagnosis
If you have tried non-surgical treatment including anti-inflammatory medication, bracing, physical therapy, activity modification, and injections, and continue to experience ankle pain and decreased function from arthritis, your foot and ankle orthopedic surgeon may recommend ankle replacement.
Ankle replacement is not recommended if you have severe deformity, dead bone in the talus (the bottom bone of the ankle joint), or bone too soft to support the joint. A history of deep infections of the ankle, significantly abnormal nerve function or sensation (also known as peripheral neuropathy), inadequate or absent leg muscle function, and poor blood flow of the leg also are signs that ankle replacement should be avoided. In these cases, an ankle fusion may be a better option for pain relief.

Post-surgery x-ray of a total ankle replacement
Treatment
Ankle replacement is performed either under general anesthesia or nerve block. Your surgeon will use a tourniquet to control bleeding and improve visualization during the surgery. They will approach the ankle from the front or the side, depending on the type of implant being used. They then cut the bone and place the metal and plastic components that recreate the ankle joint. Sometimes additional procedures will have to be done at the same time to ensure the foot and ankle are properly aligned and the deformity is corrected. Your surgeon then closes the wounds using stitches or staples, and applies a splint.
Recovery
Recovery from a total ankle replacement requires a variable period of non-weightbearing in a cast or boot to allow the implants to heal in place. The procedure is usually performed in an inpatient setting, with the patient spending up to several nights in the hospital. Strict elevation for many days after the procedure is necessary to control swelling and improve wound healing. After the surgical wounds are healed, some foot and ankle orthopedic surgeons will allow the patient to start working on gentle range-of-motion activities even if they are non-weightbearing. Weightbearing usually begins a few weeks after surgery if X-rays show good healing.
Risks and Complications
All surgeries come with possible complications, including the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. A broken bone on the side of the total ankle implant is the most common complication. Patients may also experience an injury to the tendons, nerves, or blood vessels. Wound healing is critical in the early weeks as issues with wound healing can lead to superficial or deep infections. Many of these problems are a greater risk in patients who smoke, have diabetes, or have rheumatoid arthritis. Another possible complication is the failure of the ankle implant to heal into the bone.
Just as with artificial knee and hip replacements, ankle replacements may have problems that happen even years after the initial surgery because there are moving, artificial parts. These issues may require additional surgery and include infection or loosening/wear of the artificial parts.
FAQs
There are two surgical approaches for treatment of end-stage ankle arthritis: ankle fusion and total ankle replacement. Why should I consider an ankle replacement?
There are many factors that go into this decision, so each individual case should be discussed with your foot and ankle orthopedic surgeon. In general, when motion of the ankle is preserved in an ankle replacement, the surrounding joints are protected from increased wear, which is especially important if there is already arthritis in these neighboring joints. The number of ankle replacements being performed is increasing dramatically, as is the amount of published and ongoing research in the area. Newer implant designs and improved surgical techniques constantly are evolving with the promise and goal of helping patients with an ankle replacement get results at least as good as their hip and knee counterparts.
Who should I see to have a total ankle replacement?
A foot and ankle orthopedic surgeon should be seen for management of ankle arthritis. Orthopedic surgeons who specialize in foot and ankle surgery are specifically trained to perform ankle replacements as well as take care of any complications that may arise.