The metatarsals are the long bones in the foot that connect the toes to the midfoot. The metatarsals are numbered one through five, starting with the big toe. So, the second metatarsal is the long bone of the second toe.
Second Metatarsal Shortening Osteotomy
A second metatarsal shortening osteotomy is a procedure that cuts and shortens the second metatarsal. The goals of shortening the metatarsal are to decrease pain at the base of the second toe (in the ball of the foot) and/or help straighten out the second toe.
Diagnosis
Many patients with problems have pain in the ball of their foot. Typically, they feel like they are walking on a pebble or marble. They often note more discomfort when barefoot. Many patients develop a callus (thickened skin) under the affected metatarsal head. Some patients are at risk for this due to a longer-than-normal second metatarsal.
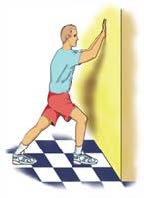
Before proceeding with this surgery, your foot and ankle orthopedic surgeon typically will try a non-surgical treatment such as a shoe insert with pads to decrease the pressure on the painful area. Note that the pad should not be placed under the painful area, but just toward the heel side of the painful area. A stretching program for the Achilles and calf muscles aimed at decreasing the pressure in the front part of the foot also can be helpful. Steroid injections should never be performed into the fat pad under the ball of the foot, but depending on the diagnosis and thought process of your surgeon, an injection may be done through the top of your foot into the joint or tissue to the side of the joint. Surgery may be an option if these initial treatments do not help. This procedure commonly is performed in combination with other procedures aimed at straightening the foot and toes and decreasing the pressure on the front part of the foot.
If you have not tried conservative treatment, you should do so before considering surgery. You should avoid this surgery if you have an infection in the foot, have poor circulation in the foot, or other medical problems that make the risks of surgery too dangerous for you.
Treatment
This surgery usually is done as an outpatient procedure, meaning the patient can go home the same day. The procedure involves cutting the second metatarsal and removing a small section of the bone. Screws and sometimes a plate are used to hold the metatarsal in the shortened position until it heals.
Specific Technique
The patient receives numbing medication for the foot along with sedation given through an IV. The foot and ankle orthopedic surgeon makes an incision on top of the foot in line with the second toe. The bone is visualized and a saw is used to make a cut in the bone. The bone is shortened to the desired length. It is held in place with some type of implant. The surgeon closes the incision and places a dressing. The surgeon also may place a splint to protect the foot. Sometimes a boot or hard-soled shoe is used.
Recovery
Your foot and ankle orthopedic surgeon will determine if you are allowed to walk or put any weight on your foot. For some patients, weightbearing is allowed the same day, but for others it may not be allowed for 6-8 weeks. The goal is to transition back to supportive shoes at 6-8 weeks based on bone healing. It can take up to 12 weeks to get back to regular shoes, and recovery time is largely determined by other procedures performed at the same time as the shortening osteotomy. The overall goal is to be 75% recovered at three months and 90-100% recovered between six and twelve months after surgery.
Risks and Complications
All surgeries come with possible complications, including the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Complications with this specific procedure can include stiffness and numbness near the incision. A delay in bone healing or a deep infection may require additional surgery.
FAQs
Why do I need to be non-weightbearing?
Depending on the specific procedure performed as well as other factors, the patient may be told to remain non-weightbearing to prevent motion between the parts of the bone that are trying to heal together. This means they should not put any weight on the affected foot. If there is too much motion between the bones it can take longer for them to heal or they may not heal at all. Bones typically take six to eight weeks to heal, so being non-weightbearing during this time should allow the bones to heal together.
What if my bones do not heal together?
This complication is more common in patients who have diabetes or smoke. This may cause continued pain after surgery, and is recognized on X-rays or CT scan. A nonunion may require a second procedure. New metal is typically placed during the second surgery and usually some form of bone graft is used to help the bones heal.