Each year millions of people in the United States-most of them children—are bitten by animals. Most animal bites are from dogs; cat bites are second most common. However, the risk of infection from a cat bite is much higher than that from a dog bite. Most bites occur on the fingers of the dominant hand, but children may also be bitten about the head and neck area.
A major concern about an animal bite is the possibility of rabies. Because most pets in the U.S. are vaccinated, most cases of rabies result from the bite of a wild animal such as a skunk, bat or raccoon. However, in other countries, dog bites are the most common source of rabies. If you are bitten by a dog outside the U.S., consult a doctor immediately.
Signs and Symptoms of Animal Bites
In some cases, the bite will not break the skin but may cause damage to underlying tendons and joints. If the skin is broken, there is the additional possibility of infection as well as injury to tendons and nerves. Dogs have powerful jaws and can cause crushing injuries to bone, muscles, tendons, ligaments and nerves.
Signs of an infection include:
- Warmth around the wound
- Swelling
- Pain
- A pus discharge
- Redness around the puncture wound
Signs of damage to tendons or nerves include:
- An inability to bend or straighten the finger
- A loss of sensation over the tip of the finger
First aid
- Don’t put the bitten area in your mouth! You will just be adding the bacteria in your mouth to that already in the wound.
- If the wound is superficial, wash the area thoroughly. Use soap and water or an antiseptic such as hydrogen peroxide or alcohol. Apply an antibiotic ointment and cover with a non-stick bandage. Watch the area carefully to see if there are signs of damaged nerves or tendons. Some bruising may develop, but the wound should heal within a week to 10 days. If it does not, or if you see signs of infection or damage to nerves and tendons, seek medical help.
- If there is bleeding, apply direct pressure with a clean dry cloth. Elevate the area. Do not clean a wound that is actively bleeding. Cover the wound with a clean sterile dressing and always seek medical help.
- If the wound is to the face and/or head and neck area, seek medical help immediately.
- Contact your physician to see whether additional treatment is needed.
- Report the incident to your public health department. They may ask your assistance in locating the animal so that it can be confined and observed for symptoms of rabies.
Medical assistance
Tell your doctor how you got the bite. Your physician will wash the wound area thoroughly and check for signs of nerve or tendon damage. The doctor may examine your arm to see if there are signs of a spreading infection. Your physician will probably leave the wound open (without stitches), unless you have a facial wound. You may need to get X-rays and a blood test. You may also need to get a tetanus shot and a prescription for antibiotics. If the tendons or nerves have been injured, you may need to see a specialist for additional treatment.
More about Rabies
Rabies is a disease that affects only mammals (such as raccoons, bats, dogs, horses, and humans). It is caused by a virus that attacks the nervous system. Without treatment, it is 100 percent fatal. Rabies develops in two stages.
During the first stage, which can last up to 10 days, the individual may have a headache, fever, decreased appetite, vomiting and general malaise, along with pain, itching, and tingling at the wound site. Symptoms of stage two include difficulty in swallowing, agitation, disorientation, paralysis, and coma. At this point, there is no known, effective treatment.
If rabies is identified early, a series of highly effective vaccinations can be administered. That’s why it’s important to capture and observe the animal that bit you. If the animal cannot be captured, but must be killed, the head should be kept intact so the brain can be examined for signs of rabies.
Preventing Animal Bites
Follow these recommendations to prevent animal bites and rabies.
- Do not try to separate fighting animals.
- Avoid animals that appear sick or act strangely. Call animal control.
- Leave animals, even pets or other animals you know, alone when they are eating or sleeping.
- Keep pets on a leash when out in public.
- Never leave a young child alone with a pet. Don’t allow children to tease an animal by waving sticks, throwing stones, or pulling a tail.
- Be sure your pet is vaccinated.
- Do not approach or play with any kind of wild animal. Teach children not to pet strange animals, even pets on a leash, without asking permission of the owner first.

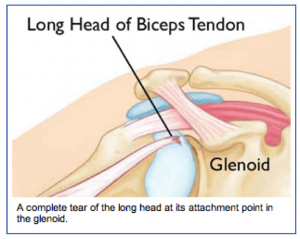 Diagnosis: The physician’s work-up will start with a careful history and exam. X-rays will be normal as they show the bones and joints, not the muscles and tendons. An MRI scan can be obtained to confirm the diagnosis, especially if the diagnosis is not obvious by history and exam.
Diagnosis: The physician’s work-up will start with a careful history and exam. X-rays will be normal as they show the bones and joints, not the muscles and tendons. An MRI scan can be obtained to confirm the diagnosis, especially if the diagnosis is not obvious by history and exam.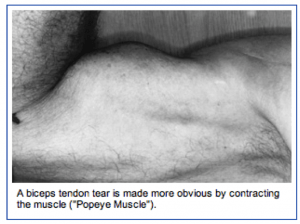 Surgery is usually accomplished through the arthroscope to remove the frayed tissue.
Surgery is usually accomplished through the arthroscope to remove the frayed tissue.