One of the more recent national trends in the fitness industry is the rise of Crossfit, and with at least 12 of these fitness gyms located throughout the city, Seattle is no exception. This is a high intensity workout method that focuses on major body movements to train multiple muscle groups simultaneously. One of the movements performed regularly by avid Crossfitters is the pull up. Of course, a strong grip on the overhead bar is required to complete this exercise, especially the “kipping” variety, where the athlete rocks the body and uses the shifting body weight to assist in the lift. With its emphasis on pull-ups as a foundational exercise, Crossfitters have started to see their share of wrist and hand injuries, one of them being trigger finger.
The hand and wrist are often susceptible to overuse injuries, especially those who perform repetitive tasks related to sports activities or various occupations. One common condition that may arise as noted above is trigger finger, which is characterized by restricted movement in one or more fingers in the hand. With this repetitive use injury the affected finger typically becomes stuck in the bent, or flexed position.
Trigger finger, medically termed stenosing tenosynovitis is an inflammation of the finger tendon sheath located in the palm of the hand and can be present in any of the fingers or even the thumb. The tendons in the hand are encased in a layer of tissue called a sheath, which allows the tendon to glide easily as the finger is bent and straightened. The action is similar to a bicycle’s brake cable sliding within the outer casing as the brake lever is depressed and then released. However, at times the sheath may become inflamed, causing a restricted gliding action.
Generally the hand will be able to close and grasp objects without difficulty, but when the fingers are straightened, the tendon will become stuck within the sheath, leaving one bent finger. The person will then usually exert more force to straighten the finger, causing the tendon to snap through the sheath and rapidly straighten. The connotation is that of the hammer on a firearm snapping closed, and is where trigger finger gets its common name.
What causes Trigger Finger?
Trigger Finger is generally caused from repetitive use of the fingers. Those individuals whose occupations require repeated and forceful grasping of tools such as tradesmen may be susceptible to this injury. Others such as rock climbers, with their forceful use of the finger flexors, are also at risk.
Clinically, I generally see this condition in those between 40-60 years of age and it is more common in women than in men. Those individuals with diabetes or rheumatoid arthritis may be at increased risk for developing trigger finger. Because it is an inflammatory condition, trigger finger usually produces local pain over the affected area in addition to the hallmark trigger effect. You may also feel a small bump in the palm of the hand where the tendon is inflamed.
The first step in treating trigger finger is to see a physician who specializes in hand injuries. Your doctor will be able to diagnose the extent of the injury and guide you toward the most effective treatments, reducing recovery time.
How is Trigger Finger Treated?
Conservative steps such as anti-inflammatory medications and rest are usually advocated initially. However, if the condition persists, I usually will treat with a steroid injection, which is a much more potent anti-inflammatory. This is a highly effective treatment modality for most patients and relief may last several months or longer. Should symptoms return after the injection wears off, surgical release of the tendon sheath may be indicated. This is a minimally invasive day surgery in which the sheath is widened, allowing the tendon to glide freely through the previously restricted area. This procedure has excellent long-term success and potential to return to 100% functional use of the hand.
There is usually a quick recovery time and post-operative physical therapy is not always needed. However, if you have had trigger finger for a long time, then there may be some underlying stiffness in the finger joints themselves. Should this be the case, I may refer you to a therapist who specializes in hand rehabilitation in order to expedite recovery and full range of motion in the hand.
Should you have any questions or concerns regarding trigger finger or any other issues concerning the hand, elbow, or shoulder, please feel free to contact my office for a consultation at (206) 633-8100 ext. 18133.
 Summers in the great Pacific Northwest brings out the adventurous side in all of us.
Summers in the great Pacific Northwest brings out the adventurous side in all of us. 
 The
The 
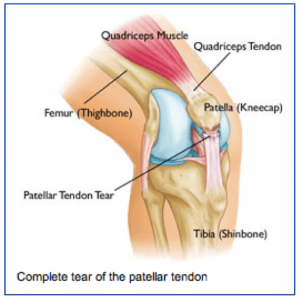 Anatomy
Anatomy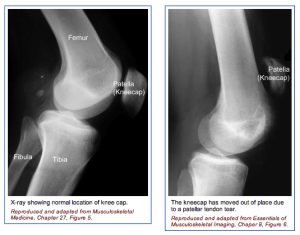 The physician’s work-up will start with a careful history and exam. The physician can often feel the defect in the patellar tendon and can appreciate the weakness on trying to straighten out the knee against resistance.
The physician’s work-up will start with a careful history and exam. The physician can often feel the defect in the patellar tendon and can appreciate the weakness on trying to straighten out the knee against resistance.