A broken thumb is a serious problem because it affects your ability to grasp items in your hand and can increase the risk of arthritis later in life.
Anatomy
The thumb has two finger bones connected to a hand bone. The first finger bone (distal phalange) extends from the tip of the thumb to the knuckle. The second finger bone (proximal phalange) extends from the knuckle to the webbing between the thumb and the first finger. There, it connects with the hand bone (first metacarpal), which extends from the webbing down to the wrist.
Although a break can occur in any of these bones, the most serious breaks happen near the joints, particularly at the base of the thumb near the wrist.
These fractures have specific names, depending on the type of break. The Bennett and Rolando fractures are breaks at the base of the thumb, involving the joint between the thumb metacarpal and a specific wrist bone. Fractures that involve the joints are always more difficult to treat and are at increased risk of an unfavorable outcome.
How it happens
Thumb fractures are usually caused by direct stress, such as when you fall or when a ball catches and pulls the thumb back. Some fractures may be caused indirectly, from twisting or muscle contractions. People who play contact sports such as wrestling, hockey or football; skiers; and people with a history of bone disease or calcium deficiency are especially at risk.
The risk of a thumb fracture can be lessened by using protective taping, padding or other equipment and by developing strength in your hands through exercise and proper nutrition.
Symptoms of a fracture
- Severe pain at the fracture site
- Swelling
- Limited or no ability to move the thumb
- Extreme tenderness
- A misshapen or deformed look to the thumb
- Numbness or coldness in the thumb
Treatment options
See a doctor as soon as possible. Without immediate treatment, the joint will be unstable and you will be unable to grip or pinch properly. Continued swelling may make it more difficult to align the bones properly. Delayed treatment will make the fracture much more difficult to treat and can lead to a poor outcome. Use a padded splint to prevent the bone from moving further out of alignment is encouraged prior to definitive treatment.
The physician will examine the injury, take your medical history and have X-rays taken of the injury. You may need surgery, depending on the location of the fracture and the amount of movement between the broken pieces of bone. If there is little movement (displacement) or if the break is located in the middle (shaft) of the bone, an orthopaedist may be able to use a specially designed cast (spica cast) to hold the bone fragments in place. You will have to wear the cast for at least four to six weeks, and your doctor may request regular X-rays to ensure that the bone hasn’t slipped out of alignment.
Often, Bennett and other more severe fractures of the thumb require surgical treatment. The hand surgeon may use one of several operative fixation techniques to restore boney anatomy and hold the bones in place while they heal. These techniques include the use of wire, pins, plates and screws as internal fixation. Another technique uses pins in bone that exit the skin and are attached to an external fixation device You will likely be required to wear a cast or splint for two to six weeks after surgery. When the cast is removed, your physician may recommend hand therapy to restore movement. It can take three months or more to regain full use of the hand, depending on the severity of the injury.
Complications and outcomes
If the bones remain in a stable position, thumb fractures generally heal well. There is a possibility of infection and tenderness around the surgical site and around the pins, if external fixation is used. As with all joint injuries, there is an increased tendency to develop arthritis, which can limit motion and reduce strength in the thumb.
To help restore motion, soak your hand in warm water and move your thumb in a circular direction. Try to touch your little finger with your thumb. To help restore strength, get a spring-type hand squeezer and use it regularly.

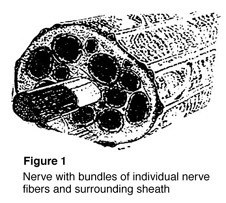 Nerves are the “electrical wiring” system in all people that carry messages from the brain to the rest of the body. A nerve is like an electrical cable wrapped in insulation. A ring of tissue forms a cover to protect the nerve, just like the insulation surrounding an electrical cable (Figure 1).
Nerves are the “electrical wiring” system in all people that carry messages from the brain to the rest of the body. A nerve is like an electrical cable wrapped in insulation. A ring of tissue forms a cover to protect the nerve, just like the insulation surrounding an electrical cable (Figure 1).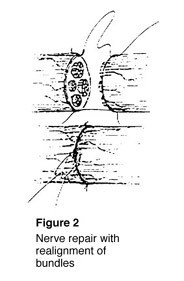 To fix a cut nerve, the insulation around both ends of the nerve are sewn together. The goal in fixing the nerve is to save the cover so that new fibers may heal and work again (Figure 2). If a wound is dirty or crushed, your physician may wait to fix the nerve until the skin has healed.
To fix a cut nerve, the insulation around both ends of the nerve are sewn together. The goal in fixing the nerve is to save the cover so that new fibers may heal and work again (Figure 2). If a wound is dirty or crushed, your physician may wait to fix the nerve until the skin has healed.