The subtalar joint is located just below the ankle joint between the talus bone and the calcaneus (heel) bone. The main job of the subtalar joint is to allow for side-to-side movement of the foot and ankle. This movement aids in walking, especially on uneven surfaces.
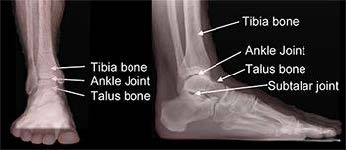
Parts of the Ankle
A fusion surgery locks bones together and is appropriate for diseased joints that can’t be replaced. Once a fusion heals together, it acts as one unit and can restore function and provide significant pain relief. Generally speaking, fusion also is very durable.
Subtalar Fusion
Subtalar fusion is performed to either correct rigid, painful deformities or instability of the subtalar joint, or to remove painful arthritis of this joint. During surgery, this joint between the talus bone above and calcaneus bone below is removed as the joint surfaces are fixed together. The goals of subtalar fusion are to decrease symptoms and allow improved function with less pain.
Diagnosis
Those with subtalar problems typically complain of pain along the outer side of the foot just below the ankle. Subtalar pain may be mistaken for ankle pain. Patients with subtalar joint problems frequently limp, favor the painless other foot, and notice swelling in this region. People commonly have difficulty and pain while walking on uneven surfaces and complain of stiffness in the foot.
Subtalar fusion generally is performed for three reasons: to correct deformity, correct instability, or treat painful arthritis. Causes of arthritis include trauma, degeneration, rheumatologic conditions, and infections.
Treatments
Your foot and ankle orthopedic surgeon will discuss your treatment options with you before proceeding with a subtalar fusion. Skin problems in the area of the surgical site, poor overall health, or active infections may cause your surgeon to delay the procedure.
Smoking increases the risk of blood clots, wound healing problems, and the possibility the fusion won’t heal. You should completely stop nicotine use at least one month before surgery and abstain until the fusion has healed. Inability or unwillingness to follow the treatment plan may mean surgery is not for you.
Specific Technique
Patients are positioned on their back or side to allow exposure of the operative leg. Subtalar fusion is most often performed through an incision on the outer side of the foot. The joint surfaces are prepared by removing all cartilage and correcting all deformity. The bone surfaces are roughened to stimulate bleeding. This bleeding allows the two bones to heal together after the joint is fixed with hardware (screws). X-rays will be used during the surgery to ensure proper alignment and hardware position. Sometimes bone graft is added to help the healing. Once surgery is finished, the foot and ankle are placed in a well-padded splint.
Recovery
After surgery, pain medication will be required for a period of time. Some people may require medication only for a day or two and others for longer. In the first few weeks after surgery you must rest and elevate the operative leg to control swelling and allow the skin incisions to heal. When upright, you may experience throbbing and discoloration in the toes as the blood rushes back to the foot, but typically this resolves with elevation. It is important to keep weight off the foot.
Once stitches are removed, there will be fewer restrictions. A boot or cast usually is placed after the initial surgical bandages are removed. The boot or cast will be in place for 8-12 weeks, sometimes longer for certain patients. Depending on your surgeon’s assessment, weightbearing may be restricted until the X-rays show healing, or weight may slowly be added throughout the period of recovery. If the surgery is on the right foot, do not plan on driving until fully healed. X-rays will be necessary until full healing is seen.
Risks and Complications
All surgeries come with possible complications, including the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
A potential complication of any fusion procedure is a failure of the fusion to heal, which is called a nonunion. Healing in a bad position also can occur, but this is rare. Following your surgeon’s instructions is very important to avoid complications.
