The Tommy John Surgery and Little Leaguer’s Elbow
With a 13-3 record during the spring and summer of 1974, Los Angeles Dodgers pitcher Tommy John was having an incredible year. Then, mid way through the season, the left-handed sinkerball thrower significantly tore through the ulnar collateral ligament (UCL) on his throwing arm. The UCL, located on the inside aspect of the elbow, comes under extreme stress during the throwing motions and it is impossible to pitch at the major league level without it intact.
The season was over for Tommy John. In fact, up until that point it could have been assumed that his entire career was over. But on September 25, 1974, Tommy became the first person to undergo reconstructive surgery that would allow him to return to the playing field for the 1976 season.
The surgery, now commonly known as Tommy John surgery, replaced the damaged ligament with a tendon from his non-throwing forearm. These days, orthopedic surgeons can take a tendon from a variety of locations, including the hamstring or Achilles tendons. Although the rehabilitation process is lengthy at about one year, athletes have a good chance of recovery. Close to 85% of throwers will be able to achieve the same level of competitiveness once the process is complete.
Tommy John surgery is performed mainly on high level throwing athletes; however, injuries to the same area can plague the younger players as well. On the other end of the spectrum is little leaguer’s elbow. This is also an injury caused by repeated stress to the ulnar collateral ligament, but the difference here is that the force of a child or adolescent pitching a baseball does not cause the ligament to break. Here, the stress leads to an uneven growth between the inside and outside aspects of the elbow. This abnormal bone development may result in cubital tunnel syndrome, which is a compression of the ulnar nerve (funny bone) as it passes through the elbow. This can in turn cause numbness, tingling, or weakness in the elbow or hand.
In some cases of little leaguer’s elbow, there may even be a stress fracture where the UCL attaches.3 The young athlete will have pain with throwing a baseball, and may be tender to the touch over the inside of the elbow. Little league baseball mitigates the risk of this condition developing by setting rest requirements and pitch count limits. All coaches and league officials should follow these regulations. If your child is a little league pitcher, you should make sure that he does not exceed the recommended limits for his age group.
Year round baseball play may also increase the risk of little leaguer’s elbow. In Seattle of course, weather does not permit youth baseball to continue year round, but some pitchers aspiring to improve their skills may seek indoor facilities to continue their practice. In this case, players should follow the guidance of the USA Baseball Medical and Safety Advisory Committee, which states that pitchers should not play for more than nine months total per year.
Pitchers certainly are at risk for arm and hand injuries, but the rest of the team is not immune from getting hurt either. Fractures to the hand may result from getting struck by a pitch while gripping a bat or sliding into a base. Diagnosing a fracture in the hand is usually done with X-ray. Treatment for simple fractures is casting for 6-8 weeks, although surgical fixation may be required for more complex breaks.
One final injury worth discussing is mallet finger, also called baseball finger. This injury is a tearing of the tendon that straightens the most distal joint of the finger. The injury mechanism is usually a “jammed finger”, either from sliding into a base or being struck on the top of the finger with a ball. The inability to fully straighten the finger will usually send the player to a physician, who can make the diagnosis through clinical presentation.
Treatment for this injury usually involves splinting the finger for several weeks. If adequate function has not been restored after splinting or if there was a bone fracture or joint misalignment during the original injury, then surgical repair may be necessary. This could consist of tendon grafting to the damaged finger, or using small pins or screws to fix bone fragments.
Wayne Mitchell Weil, MD, specializes in the surgical and non-surgical treatment of hand and elbow disorders. Dr. Weil uses the latest surgical techniques, including minimally invasive carpal and cubital tunnel releases. Those suffering from pain or reduced functional use of their hand or elbow should contact Dr. Weil for a consultation.
 We are excited to be part of the 64th annual Wallingford Family Parade and Festival on Saturday, July 6th. The parade starts at 11am and the festival follows starting at 12 pm.
We are excited to be part of the 64th annual Wallingford Family Parade and Festival on Saturday, July 6th. The parade starts at 11am and the festival follows starting at 12 pm. 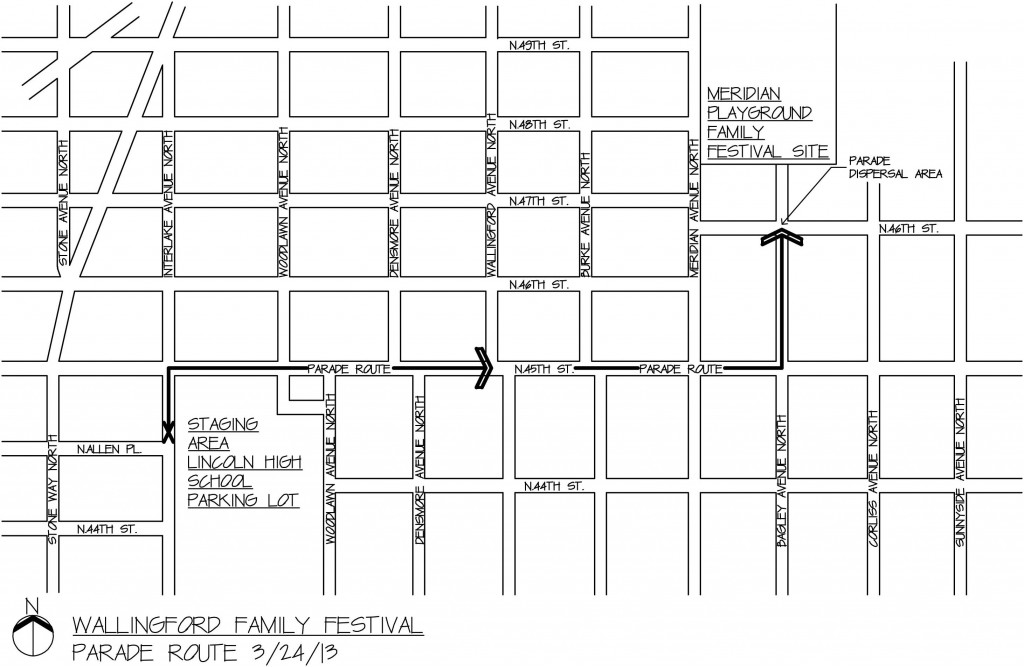

 Summers in the great Pacific Northwest brings out the adventurous side in all of us.
Summers in the great Pacific Northwest brings out the adventurous side in all of us.  The
The