From orthoinfo.aaos.org
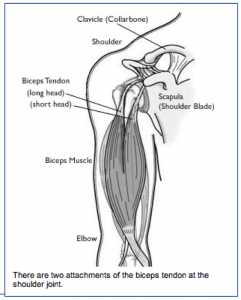
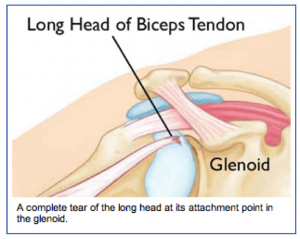
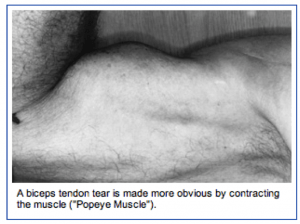
When it is torn at the upper end or at the labral attachment, there is often pain in the front of the shoulder. When the long head of the biceps is completely torn, the biceps muscle has a typical bulging appearance, but oftentimes does not cause much discomfort of weakness.
Injury Mechanism: Acute injuries to the long head of the biceps occur with heavy lifting or by grabbing the railing to support one’s body weight during a fall. Tears of the biceps can also occur with repetitive use of the shoulder in sports or work.
Symptoms: Acute complete tears of the long head of the biceps usually present as a sharp pain in the front of the shoulder, followed by bruising and the “Popeye muscle” deformity of the biceps (bulging in the middle of the upper arm where the muscle has retracted). Chronic tears or fraying of the biceps usually presents as aching in the front of the shoulder with use of the biceps.
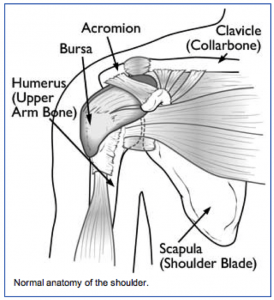
 Diagnosis: The physician’s work-up will start with a careful history and exam. X-rays will be normal as they show the bones and joints, not the muscles and tendons. An MRI scan can be obtained to confirm the diagnosis, especially if the diagnosis is not obvious by history and exam.
Diagnosis: The physician’s work-up will start with a careful history and exam. X-rays will be normal as they show the bones and joints, not the muscles and tendons. An MRI scan can be obtained to confirm the diagnosis, especially if the diagnosis is not obvious by history and exam.
Treatment: Your physician will discuss treatment options with you. Most complete tears of the rotator cuff can be treated without surgery. Rarely patients notice weakness or cramping in the biceps. Stretching, strengthening, anti-inflammatories, and time will usually settle down symptoms to a tolerable level.
The partial tears are usually more painful. Injections can sometimes manage the discomfort, but occasionally surgery is necessary to help alleviate symptoms.
 Surgery is usually accomplished through the arthroscope to remove the frayed tissue.
Surgery is usually accomplished through the arthroscope to remove the frayed tissue.
If the partial tear is nearly complete, the tendon is released from its attachment to the socket (labrum) and attached further down on the upper arm bone (humerus). This procedure is called a biceps tenodesis. Sometimes a small incision is necessary to re-attach the tendon to the bone.
What to expect after surgery: If the frayed tendon is just removed through the arthroscope, the recovery is rapid. Usually, after a few days of rest, gentle exercise is started. A full recovery is expected after 4 to 6 weeks. If the tendon is re-attached to bone, a sling is used with the elbow bent for 3 or 4 weeks to protect the repair. No resisted use of the biceps is started until 6 to 8 weeks after the repair.

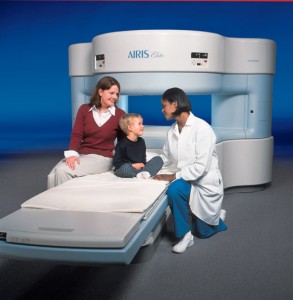 The result of our OPEN MRI is a sophisticated diagnostic picture of the area your orthopedic specialist wishes to view. What’s more, there is no pain, no known side effects, and no radiation used with our OPEN MRI.
The result of our OPEN MRI is a sophisticated diagnostic picture of the area your orthopedic specialist wishes to view. What’s more, there is no pain, no known side effects, and no radiation used with our OPEN MRI.